Symptomatic bradycardia occurs when the heart rate drops below 50 beats per minute.
Most often, a significant slowing of the heart rate stems from dysfunction in the heart’s conduction system, particularly high-degree blockages. These blockages can result from impaired impulse generation in the sinoatrial node or disrupted conduction from the sinoatrial node to the atria (sinoauricular) or ventricles (atrioventricular).
A notable decrease in heart rate often leads to compromised blood supply to organs and systems, especially the heart and brain. This can contribute to the development of acute heart failure, myocardial ischemia, and impaired mental status.
Causes of occurrence
- Internal Causes:
- Idiopathic degenerative fibrosis (most common).
- Myocardial ischemia.
- Myocarditis (especially associated with Lyme disease, diphtheria, and rheumatic fever) and pericarditis.
- Cardiomyopathy.
- Infiltrative diseases (such as sarcoidosis, hemochromatosis, and amyloidosis).
- Collagen disorders (rheumatoid arthritis, scleroderma, systemic lupus erythematosus).
- Congenital heart defects.
- Genetic mutations (e.g., SCN5A, TRPM4, and others).
- Surgical interventions on the heart (such as heart valve replacement, Maze procedure, aorto-coronary bypass, and others).
- Heart irradiation.
- External Causes:
- Medications (such as digoxin, beta-blockers, calcium channel antagonists, ivabradine, clonidine, reserpine, class I and III antiarrhythmic drugs, antidepressants, narcotic drugs, lithium drugs, cannabinoids, cimetidine).
- Vagotonia (during night sleep, endotracheal aspiration, strong cough, urination, and other activities).
- Hypersensitivity of the carotid sinus.
- Endocrine disorders (e.g., hypothyroidism).
- Electrolyte disturbances (including hyperkalemia, hypokalemia, hypercalcemia, hypermagnesemia).
- Hypothermia, hypoxemia, hypercapnia, anorexia, acidosis.
- Neurological disorders (such as trauma or tumor of the central nervous system accompanied by increased intracranial pressure).
- Obstructive sleep apnea syndrome.
- Chest injury.
Clinical presentation
Most patients with sinus bradycardia are asymptomatic.
Symptoms typically arise when the heart rate drops below 50 beats per minute.
The clinical presentation of symptomatic bradycardia can vary, ranging from mild fatigue, dizziness, and reduced tolerance to physical exertion, to hypotension, signs of acute heart failure, chest discomfort, and loss of consciousness.
Medical history
Careful collection of anamnestic data is crucial for determining the cause of bradycardia.
- Inquire about the onset and nature of symptoms, including factors that may have triggered them such as stress, physical exertion, medication, or food intake.
- Determine if the patient sought prior medical assistance and if so, the outcome of the consultation.
- Assess if the patient self-administered any medications and whether this affected the nature of their symptoms.
- Review any prior hospitalizations for symptomatic bradycardia, focusing on clinical diagnoses, laboratory or instrumental findings, treatment, and post-discharge recommendations.
- Analyze previous laboratory or instrumental examinations related to the current complaints for relevant findings.
- Understand the patient’s motivation for seeking your assistance.
- Rule out alternative causes of symptoms through targeted questioning.
- Ascertain any history of cardiovascular diseases, including myocardial infarction, angina pectoris, cardiomyopathy, congenital heart defects, and myocarditis.
- Determine if the patient has been diagnosed with rhythm or conduction disorders previously.
- Inquire about any infiltrative diseases, connective tissue disorders, endocrine diseases, or neurological conditions associated with increased intracranial pressure.
- Obtain information on previous surgical procedures, particularly those involving prosthetic heart valves, aorto-coronary bypass, or the Maze procedure, and inquire about postoperative recovery.
- Document current medication use, including doses, especially medications such as digoxin, beta-blockers, calcium channel blockers, antiarrhythmics, and electrolyte supplements.
- Investigate recent infectious diseases or tick bites.
- Assess the patient’s family history of cardiovascular disease, including rhythm or conduction disorders.
Physical examination
The primary objective sign of symptomatic bradycardia is a heart rate (HR) slower than 60 beats per minute, which may be the sole indicator in some cases.
When the heart rate moderately decreases, blood pressure typically remains within normal limits. However, a significant drop in heart rate often leads to hypotension.
A substantial reduction in heart rate can manifest with signs of acute heart failure, including moist wheezing in the lungs, tachypnea, and cyanosis.
Diminished blood supply to the brain may result in altered consciousness.
Furthermore, during physical examination, it is essential to search for signs indicative of the underlying disease causing the bradycardia.
Additional examination methods
Plan of laboratory examination methods:
- Blood analysis for electrolyte levels.
- Thyroid hormone and TSH blood tests.
- Complete blood count.
- Coagulation profile (coagulogram).
- Blood tests for creatinine and urea levels.
- Troponin-I blood test.
- Blood tests for IgM and IgG antibodies to Borrelia (Lyme disease).
- PCR for detection of Borrelia DNA.
- Assessment of blood pH.
- Genetic testing.
- Toxicological screening
Plan of instrumental survey methods :
- Electrocardiography (ECG) in 12 leads.
- Transthoracic echocardiography.
- Ambulatory ECG monitoring (Holter monitoring).
- ECG stress test.
- Coronary angiography.
- Cardiac magnetic resonance imaging (MRI).
- Positron emission tomography (PET scan).
- Electrophysiological study.
- Polysomnography (sleep study).
Laboratory tests that should be performed in patients with cardiac conduction disorders include a blood test for electrolytes, a blood test for the level of thyroid hormones, a blood test for troponin-I/T when acute myocardial ischemia is suspected, and a serological test for Borrelia antibodies when suspected for Lyme disease, determination of the blood pH level in case of suspicion of metabolic acidosis, determination of the level of digoxin in the blood in case of suspicion of glycoside intoxication.
- Electrocardiography in 12 leads
ECG in 12 leads is essential for evaluating all patients with symptomatic bradycardia. If characteristic changes are not evident on resting ECG, ambulatory ECG monitoring is advisable.
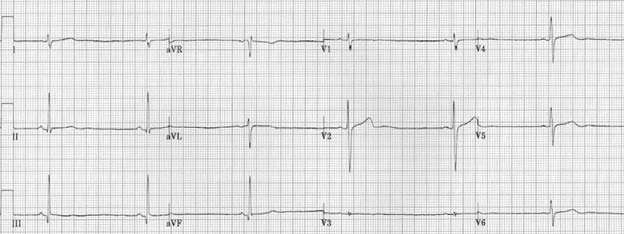
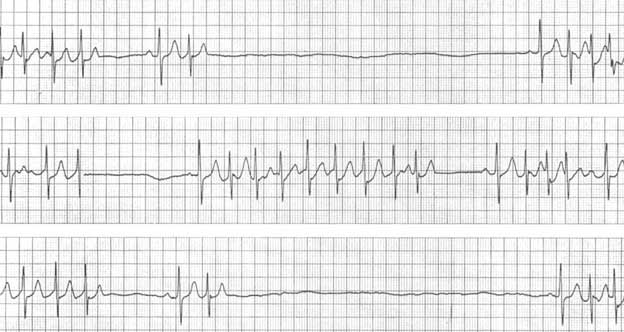
Persistent sinus bradycardia is diagnosed when the heart rate remains below 50 beats per minute persistently (see Figure 1).
Figure 1. Persistent sinus bradycardia. Image from litfl.com internet resource. https://litfl.com/sinus-bradycardia-ecg-library
Manifestations of sinus node weakness syndrome include: persistent sinus bradycardia, ectopic atrial bradycardia, sinoatrial blockade of various degrees, pacemaker migration, sinus node arrest with a pause lasting more than 3 seconds, bradysystolic form of atrial fibrillation, tachy-brady syndrome, chronotropic incompetence, isorhythmic dissociation .
AV blocks are characterized by prolongation of the PQ interval with or without loss of ventricular complexes.
- ECG with dosed exercise
A timed exercise ECG may be beneficial for patients experiencing symptoms of bradycardia during or immediately after exercise. Appearance of bradycardia symptoms during exercise typically indicates cardiac pathology, whereas occurrence immediately after physical activity suggests a reflex mechanism.
Additionally, an ECG test with dosed physical load is essential to detect chronotropic incompetence, a manifestation of sinus node weakness syndrome. An inadequate chronotropic response of the sinus node (less than 80% of the expected maximum heart rate) during exercise is indicative of sinus node dysfunction.
- Visualizing examination methods
Echocardiography is recommended for all patients with symptomatic bradycardia to assess for possible structural heart disease, evaluate left ventricular systolic function, and diagnose any underlying causes that may have led to cardiac conduction abnormalities
- Coronary angiography or CT angiography is recommended if coronary heart disease is suspected.
- MRI
MRI of the heart is highly informative for diagnosing myocardial inflammation or fibrosis, particularly in patients under 60 years of age, where suspicion of such conditions arises.
- Genetic testing
In most cases, heart conduction disorders arise due to age-related or structural changes in the heart’s conduction system. However, mutations in genes such as SCN5A, TRPM4, and LMNA can also be responsible for heart blocks. Current understanding suggests that mutations in these genes lead to a progressive conduction system disease, particularly in young patients under the age of 50, even with structurally normal hearts and without signs of skeletal myopathy.
As a result, genetic testing is recommended for young patients under 50 with progressive conduction system disease.
- Polysomnography
Polysomnography is recommended for patients experiencing nocturnal episodes of bradycardia, which may be potentially associated with episodes of nocturnal sleep apnea. Hypoxemia, commonly observed in sleep apnea, can increase vagal nerve tone and contribute to the development of bradycardia.
- Electrophysiological research
An electrophysiological study is conducted in patients when the cause of bradycardia cannot be identified through non-invasive methods.
Differential diagnosis
Standard electrocardiography is typically adequate for diagnosing heart conduction disturbances, although differentiation of potential underlying causes may be necessary.
To aid in the memorization of the main causes of bradycardia, an English-language mnemonic called ‘Hs/Ts’ is often used. This mnemonic represents the initial letters of pathological conditions associated with significant slowing of the heart rate.
| H-Hypoxia | hypoxia | shortness of breath, tachypnea, cyanosis, low blood oxygen saturation |
| H-Hydrogen ion | excess hydrogen ions (acidosis) | low QRS amplitude on the ECG |
| H-Hypokalemia | hypokalemia | hypokalemia, flat T waves on the ECG, the appearance of a U wave |
| H- Hyperkalemia | hyperkalemia | hyperkalemia, high-amplitude T waves on the ECG, widening of QRS complexes |
| H-Hypothermia | hypothermia | staying in conditions of low temperatures, low body temperature |
| T-Tension pneumothorax | tension pneumothorax | progressive difficulty breathing, shortness of breath, tachypnea, cyanosis, X-ray signs of air accumulation in the pleural cavity |
| T- Tamponade | cardiac tamponade | Beck’s triad – enlargement of jugular veins, deafness of heart sounds, hypotension; fluid accumulation in the pericardial cavity |
| T-Toxins | toxins | As a rule, a prolonged QT interval is registered on the ECG; neurological symptoms may be observed |
| T-Thrombosis | thrombosis (myocardial infarction) | increased markers of myocardial necrosis, ECG signs of acute myocardial ischemia, angiographic confirmation of coronary artery occlusion |
The most common causes of life-threatening bradycardia include hyperkalemia, myocardial ischemia, and overdose with cardiac glycosides, beta-blockers, and calcium channel antagonists.
Now, let’s delve deeper into the causes of dysfunction in the heart’s conduction system, which are associated with significant slowing of the heart rate.
Sinus node weakness syndrome
Sinus node weakness syndrome is a condition characterized by dysfunction in the normal functioning of the sinus node, resulting in bradycardia and the potential development of heart failure.
This syndrome encompasses various manifestations, including:
- Persistent sinus bradycardia
- Ectopic atrial bradycardia
- Sinoatrial block of varying degrees
- Rhythm driver migration
- Sinus node arrest with pauses lasting more than 3 seconds
- Atrial fibrillation with a low ventricular contraction frequency (bradysystolic form)
- Tachy-brady syndrome (alternating episodes of tachycardia and bradycardia)
- Chronotropic incompetence (the heart’s inability to increase heart rate in response to increased activity or demand, often indicated by failure to reach 80% of expected heart rate reserve during exercise)
- Isorhythmic dissociation (where the frequency of atrial depolarization is lower than that of ventricular depolarization).
Clinical presentation
Sinus node weakness syndrome predominantly affects the elderly population, but it can also occur in individuals of all age groups.
Symptoms of sinus node weakness syndrome arise from decreased cardiac output and hypoperfusion of internal organs.
The clinical presentation of sinus node weakness syndrome can vary widely, ranging from mild fatigue, dizziness, and shortness of breath during physical exertion to reduced exercise tolerance, chest pain, and sudden loss of consciousness (Morganhi-Adams-Stokes syndrome).
Diagnostics
- ECG
The primary method for diagnosing sinus node weakness syndrome is through an ECG.
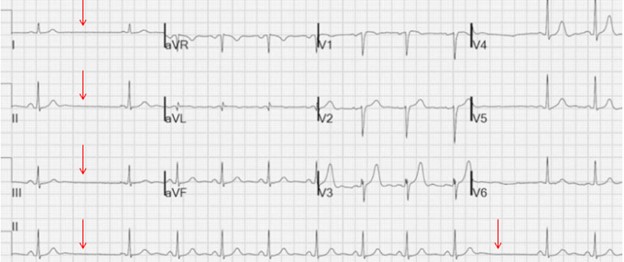
ECG findings indicative of second-degree sinoatrial block include periodic loss of the PQRST complex, with the duration of the pause equal to the sum of two or more normal RR complexes of the main rhythm (see Figure 2). Substitute complexes from the AV node or ventricles may appear during these pauses.
Figure 2. Second-degree sinoatrial block. Image sourced from the internet resource litfl.com. Accessed on https://litfl.com/sinoatrial-exit-block-ecg-library
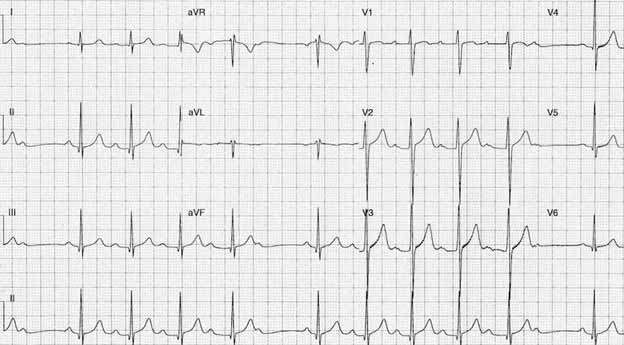
Complete sinoatrial block is characterized by a complete cessation of impulse conduction from the sinus node to the right atrium. Instead of a sinus rhythm, a substitute rhythm typically arises on the ECG, originating from secondary or tertiary pacemaker centers, most commonly the AV node (see Figure 3).
Figure 3. Complete sinoatrial block. Image sourced from the internet resource litfl.com. https://litfl.com/sinus-node-dysfunction-sick-sinus-syndrome
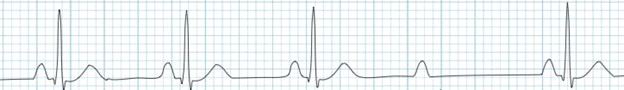
Rhythm driver migration refers to the gradual movement of the pacemaker site. This phenomenon is characterized by a gradual change in the shape and polarity of the P wave from cycle to cycle, as recorded on the ECG (see Figure 4).
Figure 4. Migration of the pacemaker. Image https://therapy.odmu.edu.ua/ecg-online-course/wandering-pacemaker
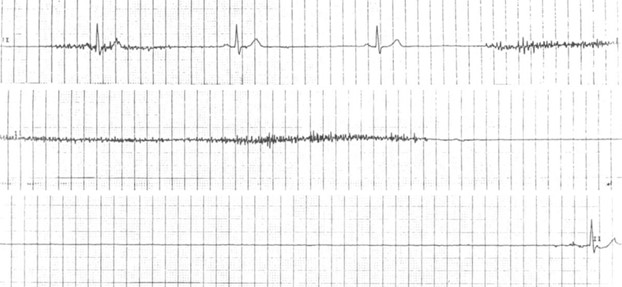
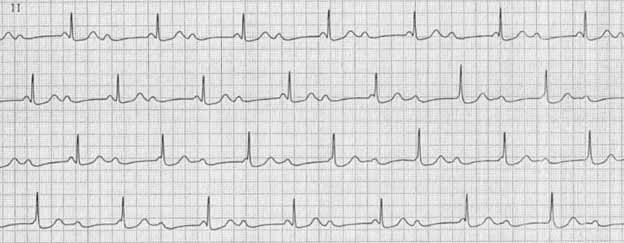
Tachy-brady syndrome is characterized by alternating episodes of tachycardia and bradycardia (Figure 5).
Figure 5. Tachy-brady syndrome. Image from litfl.com internet resource. https://litfl.com/sinus-node-dysfunction-sick-sinus-syndrome
Isorhythmic dissociation is characterized by a slower atrial depolarization originating from the sinus node or ectopic atrial region compared to ventricular depolarization originating from the AV node, His bundle, or ventricular region.
Atrioventricular blockade
Atrioventricular block refers to a partial or complete interruption of impulses’ conduction from the atria to the ventricles.
There are three degrees of AV block:
- First-degree AV block is characterized by slightly slowed conduction through the AV node, but each atrial impulse reaches the ventricles.
- Mobitz I, or second-degree AV block, involves progressive deterioration of conduction through the AV node with periodic blockade of atrial impulses.
- Mobitz II, or second-degree AV block, features persistent significant slowing of conduction through the AV node with periodic blockade of atrial impulses.
- Third-degree, or complete, AV block is characterized by complete cessation of atrial impulse transmission to the ventricles.
Symptomatic bradycardia commonly occurs in patients with second- and third-degree AV block.
Clinical Presentation:
The clinical presentation of second-and third-degree AV block can vary, ranging from mild fatigue, dizziness, reduced exercise tolerance, and dyspnea during physical exertion to loss of consciousness (Morganhi-Adams-Stokes syndrome).
Morganhi-Adams-Stokes syndrome results from cerebral ischemia due to a sudden decrease in cardiac output. Symptoms typically appear 3-10 seconds after blood circulation ceases, last several minutes, and generally do not lead to acute neurological complications
Diagnostics
- ECG
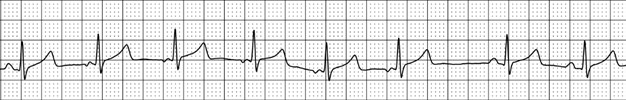
Mobitz I, or second-degree AV block, is characterized by a progressive lengthening of the PQ interval on the ECG, leading to periodic loss of QRS complexes (see Figure 6).
Figure 6. Second-degree AV block, Mobitz I. Image sourced from litfl.com. https://litfl.com/av-block-2nd-degree-mobitz-i-wenckebach-phenomenon
Mobitz II degree II AV block is characterized by persistent prolongation of the PQ interval with periodic loss of QRS complexes (Figure 7).
Figure 7. Second-degree AV block, Mobitz II. Image sourced from litfl.com internet resource. https://litfl.com/av-block-2nd-degree-mobitz-ii
Third-degree AV block is characterized by complete dissociation of atrial and ventricular waves on the ECG, with the atrial contraction frequency significantly exceeding the frequency of ventricular activation (see Figure 8).
Figure 8. Third-degree AV block. Image sourced from litfl.com internet resource. https://litfl.com/av-block-3rd-degree-complete-heart-block
Action algorithm for symptomatic bradycardia
- Maintain airway patency.
- Provide oxygen therapy in cases of hypoxemia.
- Monitor heart rate and blood pressure.
- Establish intravenous access.
- Identify and address potential causes of symptomatic bradycardia (discontinue medications and administer antidotes if available, consider myocardial revascularization for ischemic heart disease, and correct electrolyte imbalances such as hyperkalemia).
- Initiate drug treatment if hypotension, altered mental status, acute heart failure, or chest discomfort persists despite initial measures.
- Administer 0.1% atropine solution intravenously at a dose of 1.0 mg, with repeated doses every 3-5 minutes if necessary (maximum total dose: 3 mg).
- If atropine is ineffective, consider dopamine infusion at a rate of 5-20 μg/kg/min or epinephrine infusion at a rate of 0.02-0.2 μg/kg/min.
- If medical treatment is ineffective, consider percutaneous pacing.
- Note that atropine is contraindicated in patients after heart transplantation. In such cases, or in the presence of AV block due to acute myocardial ischemia, consider administering an infusion of aminophylline at a dose of 6 mg/kg or theophylline at a dose of 300 mg intravenously.
It should be noted that atropine is contraindicated in patients after heart transplantation. In such cases, as well as in instances of AV blockade occurring against the background of acute myocardial ischemia, it is advisable to administer an infusion of aminophylline at a dose of 6 mg/kg or theophylline at a dose of 300 mg intravenously.
Specific therapy is used for heart conduction disturbances caused by drug overdose:
- In cases of overdose with calcium channel antagonists:
- Calcium chloride can be administered intravenously at a dose of 1-2 g every 10-20 minutes, or as an IV infusion at a dose of 0.2-0.4 ml/kg/h.
- Alternatively, calcium gluconate can be administered intravenously at a dose of 3-6 g every 10-20 minutes, or as an IV infusion at a dose of 0.6-1.2 ml/kg/hour.
- In cases of overdose with calcium channel antagonists or beta-blockers:
- Glucagon can be administered intravenously at a dose of 3-10 mg as an IV drip, at a rate of 3-5 mg/h.
- Intravenous insulin therapy can also be considered at a dose of 0.5 IU/kg/hour.
- In cases of digoxin overdose:
- Digibind can be administered at a dose of 1 vial to bind 0.5 mg of digoxin.
Electrocardiostimulation
Temporary electrocardiostimulation is indicated for symptomatic patients with bradycardia if medical treatment fails to improve symptoms.
For long-term therapy of symptomatic bradycardia, including sinus node weakness syndrome, second-degree AV block (Mobitz type II), and third-degree AV block, permanent cardiostimulation is recommended.
The choice of cardiac stimulation type depends on the required stimulation frequency and the presence of concomitant pathology:
- For infrequent stimulation needs or in the presence of severe concomitant pathology, single-chamber ventricular cardiostimulation is advised.
- For frequent stimulation needs without severe concomitant pathology and normal AV conduction, single-chamber atrial cardiostimulation is recommended.
- For frequent stimulation needs without severe concomitant pathology but with impaired AV conduction, two-chamber cardiostimulation is recommended.
Prognosis:
With appropriate treatment, the prognosis for patients undergoing electrocardiostimulation is generally favorable. However, outcomes may vary depending on the underlying cardiac condition and any associated comorbidities.

Responses