Counseling of a patient with symptomatic bradycardia – OSCE guide
The onset of the consultation
- Wash hands and put on PPE if necessary.
- Introduce yourself to the patient by stating your name and role.
- Confirm the patient’s last name, first name and date of birth.
- Explain what the examination will involve using language the patient can understand.
- Get consent for consultation.
- Adequately expose the patient for examination.
- Ask the patient if he is in pain before proceeding with the clinical examination.
Clarification of the main complaint
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
- Analyze the patient’s thoughts, fears, and expectations
- Summarize the patient’s complaints
Comprehensive assessment
- Assess other symptoms to get a comprehensive picture
Medical history
- Find out when and how complaints first appeared; specify the possible reason for the appearance of these complaints; detailed identification of the circumstances that preceded bradycardia, for example, stress, physical exertion, taking medication or food; did the patient seek medical help, if so, to whom and how did his appeal end, if not, then specify why he did not seek medical help; whether the patient took medical drugs independently or as prescribed by the doctor, if so, whether the nature of the complaints changed
- In case of a history of hospitalization due to symptomatic bradycardia, read the extract from the patient’s medical history, pay attention to the established clinical diagnosis, the results of the laboratory or instrumental examinations, the treatment and recommendations after discharge
- If the patient has previously undergone laboratory or instrumental examinations for current complaints, analyze their results and indicate important findings
- Find out what prompted the patient to contact you
- Exclude other causes of existing complaints by asking the patient clarifying questions
History of life
- Clarify whether the patient has previously been diagnosed with cardiovascular diseases, in particular myocardial infarction, angina pectoris, cardiomyopathy, congenital heart defects, myocarditis
- Find out if the patient has previously been diagnosed with a rhythm and/or conduction disorder
- Find out whether the patient suffers from infiltrative diseases, in particular sarcoidosis, hemochromatosis, amyloidosis; systemic diseases of connective tissue, such as rheumatoid arthritis, scleroderma, systemic lupus erythematosus; endocrine diseases, in particular hypothyroidism; neurological diseases accompanied by increased intracranial pressure
- Find out if the patient has had previous surgical interventions, including prosthetic heart valves, coronary artery bypass grafting, Maze procedure, and find out how the post-operative period was
- Find out whether the patient is taking medications, in particular digoxin, beta-adrenergic blockers, calcium channel antagonists, antiarrhythmics, potassium, magnesium, calcium preparations; specify the doses of the drugs
- Find out if the patient has recently had an infectious disease and if the patient has been bitten by a tick
- Find out if the patient has a drug or food intolerance and how it manifests itself
- Find out if the patient has bad habits – drinking alcohol, drugs, smoking
- Determine whether the patient’s blood relatives have had cardiovascular disease, including rhythm and/or conduction disorders
- Find out the patient’s marital status, living conditions
- Clarify whether the patient works, his profession, working conditions, the presence of harmful occupational factors
Objective examination
- Assessment of the patient’s general condition
- Conducting a general inspection
- Evaluation of the constitution
- Estimation of the degree of obesity
- Skin and mucous membranes
- Evaluation of thyroid glands
- Assessment of peripheral lymph nodes
- Assessment of respiratory organs
- Evaluation of the cardiovascular system
- Assessment of abdominal organs
- Evaluation of organs of the genitourinary system
Laboratory examination
- Blood analysis for electrolytes
- Blood test for thyroid hormones and TSH
- Clinical blood count (if needed)
- Coagulogram (if necessary)
- Blood test for creatinine and urea (if needed)
- Blood test for troponin- I (if necessary)
- Blood test for IgM and IgG antibodies to Borrelia (if necessary)
- PCR for Borrelia burgdorferi DNA detection (if necessary)
- Assessment of blood pH (if necessary)
- Genetic testing (if needed)
- Toxicological screening (if necessary)
Diagnostic tests
- Electrocardiography in 12 leads
- Transthoracic echocardiography
- Ambulatory ECG monitoring (if necessary)
- ECG test with dosed exercise (if necessary)
- Coronary angiography (if necessary)
- MRI of the heart (if necessary)
- Positron emission tomography (if necessary)
- Electrophysiological examination (if necessary)
- Polysomnography (if necessary)
Making a clinical diagnosis
- Identification of the underlying disease
- Indication of the nature of the conduction disturbance that caused the bradycardia
- Indication of comorbid pathology
Specialist consultations
- Cardiologist
- Cardiac surgeon
- Arithmologist
- Rheumatologist
- Neuropathologist _
- Endocrinologist
- Nephrologist
- Geneticist
- Infectious Disease Specialist
Treatment
- Emergency therapy
- Long-term therapy (permanent cardiac stimulation)
Explain the procedure for cardiac stimulation
- Check the patient’s understanding of the reason for the procedure
- Check the patient’s understanding of the procedure
- Inform about the stages of the procedure
- Tell about the risks and complications
- Carry out work on mitigating fears
- Suggest an additional source of information
Consulting and support
- Inform the patient about the disease
- Explain to the patient the possible causes of the disease
- Inform the patient of the symptoms that may occur with the identified disease
- Discuss the results of the examinations with the patient
- Explain to the patient the possible consequences of the disease
- Educate the patient about available treatments
- Help the patient understand the risks and benefits of different treatments
- Answer the patient’s questions
- Provide an explanation of the extent of monitoring during and after treatment
- Schedule regular check-ups and follow-up to assess the effectiveness of treatment and changes in the patient’s condition
Monitoring the effectiveness of treatment
- Clinical assessment
- Instrumental assessment
- Control over side effects of therapy
End of consultation
- Summarize the data and ask the patient if anything important has been missed
- Inform the patient about further tactics
- Thank the patient
- Dispose of PPE properly and wash hands
Key communication skills
- Active listening
- Summing up
- Selection of indicative signs
The beginning of the consultation
- Wash hands and put on PPE if necessary.
- Introduce yourself to the patient by stating your name and role.
- Confirm the patient’s last name, first name, and date of birth.
- Explain what the examination will involve using language the patient can understand.
- Get consent for consultation.
- Adequately expose the patient for examination.
- Ask the patient if he is in pain before proceeding with the clinical examination.
Symptoms of bradycardia typically manifest when the heart rate falls below 50 beats per minute, often indicating signs of hypoperfusion in critical organs such as the brain and heart.
Clinical signs may include:
- Symptoms indicative of cerebral hypoperfusion (e.g., dizziness, blurred vision, loss of consciousness).
- Manifestations of compromised cardiac perfusion (e.g., chest pain, dyspnea, sensation of air insufficiency, diminished tolerance to physical exertion).
- General symptoms suggestive of inadequate blood supply to other organs and systems (e.g., weakness, heightened fatigue).
Clarification of the main complaint
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
- Analyze the patient’s thoughts, fears, and expectations
- Summarize the patient’s complaints
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
The most common complaints of a patient experiencing bradycardia often involve dizziness and potential loss of consciousness.
To further investigate complaints of dizziness, consider the following algorithm:
- Circumstances preceding the onset of dizziness: Inquire about recent physical activity, body position changes, emotional stressors, food or drink consumption, and medication intake.
- Onset: Determine if the dizziness occurs suddenly or develops gradually.
- Description: Prompt the patient to articulate the sensations experienced during the episode of dizziness.
- Intensity: Ask the patient to rate the severity of their dizziness on a scale from 0 to 10.
- Associated symptoms: Inquire about any additional symptoms accompanying the dizziness.
- Duration: Establish whether the dizziness occurs periodically or persists continuously.
- Aggravating or alleviating factors: Identify any factors that exacerbate or relieve the intensity of dizziness, particularly changes in body position.
“Could you describe what happened before you started feeling dizzy?”
“Does the dizziness come on suddenly or does it develop gradually?”
“Can you please explain what sensations you experience when you feel dizzy?”
“On a scale from 0 to 10, how would you rate the severity of your dizziness?”
“Are there any other symptoms that occur along with the dizziness?”
“Does the dizziness occur constantly or does it happen periodically?”
“Are there any factors that make the dizziness worse or better?”
If the main complaint of your patient is an episode of loss of consciousness, follow this algorithm:
- Circumstances preceding loss of consciousness: physical activity, prolonged standing, change in body position, emotional stress, intake of food or medication, intense cough.
- Start: Find out if any symptoms preceded the loss of consciousness (dizziness, visual disturbances, sweating, nausea, palpitations, shortness of breath).
- Concomitant symptoms: Ask the person who witnessed the fainting episode if the fainting episode was accompanied by other symptoms (including convulsions, involuntary defecation or urination).
- Duration: Ask the witness about the duration of the episode of unconsciousness.
- Factors contributing to faster recovery of consciousness: horizontal position of the body, use of medication.
“Tell me what you were doing before you lost consciousness?”
“Tell me, was loss of consciousness preceded by dizziness, sweating, nausea, palpitations, shortness of breath?”
“How long was the patient unconscious?”
“Was the episode of unconsciousness accompanied by other symptoms?”
“Was there anything that helped you to restore the consciousness of the patient?”
Analyze the patient’s thoughts, fears, and expectations
A key component of history-taking is exploring the patient’s thoughts, concerns, and expectations to gain insight into how the patient currently perceives their condition, their concerns, and what they expect from the consultation.
The exploration of thoughts, concerns, and expectations should be fluid throughout the consultation in response to cues from the patient. This will help to make your consultation patient-oriented, rather than formulaic.
It is essential to structure the analysis of thoughts, fears, and expectations so that it sounds natural in your consultation.
| Reflections | Explore the patient’s perception of the current problem | “What do you think could have caused these symptoms?” “Do you have any ideas about why these symptoms appeared?” |
| Concern | Explore the patient’s current concerns | “Is there something specific that’s been bothering you?” “How do you usually manage your daily activities?” “Is there anything else you feel we should talk about?” |
| Expectation | Ask what the patient hopes to gain from the consultation | “How can I assist you during today’s consultation?” “What are you hoping to achieve from today’s appointment?” “In your opinion, what would be the most suitable approach moving forward?” |
Summarize the patient’s complaints
Summarize the patient’s complaint to ensure understanding and provide an opportunity for the patient to correct any inaccuracies. After summarizing, ask if there’s anything else the patient would like to add or clarify. Throughout the consultation, periodically summarize intermediate findings
Comprehensive assessment
- Screen for symptoms of damage to other organs and systems
A comprehensive assessment involves briefly surveying the patient for symptoms of other systems, which may or may not be related to the chief complaint. This approach can help identify symptoms the patient may have overlooked.
Here are some examples of symptoms to monitor for each system:
| System | Symptoms |
| General manifestations | fever, weight change, fatigue, sweating, general weakness |
| Respiratory | shortness of breath, cough, sputum discharge, wheezing, hemoptysis, pleural chest pain |
| Cardiovascular | chest pain, shortness of breath, swelling of the lower extremities, heart failure |
| Gastrointestinal | dyspepsia, nausea, vomiting, dysphagia, abdominal pain, stool disorders |
| Genitourinary | oliguria, polyuria, nocturia, pain during urination |
| Neurological | vision changes, motor or sensory disturbances, headache, paresis, plegia |
| Locomotor | pain in the chest wall, bone pain, trauma |
| Skin | rashes, ulcers, hemorrhages, petechiae, bruises, hemorrhages, neoplasms |
Medical history
- Find out when and how complaints first appeared; specify the possible reason for the appearance of these complaints; did the patient seek medical help, if so, to whom and how did his appeal end, if not, then specify why he did not seek medical help; whether the patient took medical drugs independently or as prescribed by the doctor, if so, whether the nature of the complaints changed
“When did you first experience these symptoms?”
“What do you think might be causing these symptoms?”
“Have you consulted a healthcare professional about this issue?”
- In case of a history of hospitalization due to symptomatic bradycardia, read the patient’s medical history, pay attention to the established clinical diagnosis, the results of the laboratory or instrumental examinations, the treatment and recommendations after discharge
- If the patient has previously undergone laboratory or instrumental examinations for current complaints, analyze their results and indicate important findings
- Find out what prompted the patient to contact you
“What led you to reach out to me?”
“What prompted you to seek my assistance?”
- Exclude other causes of existing complaints by asking the patient clarifying questions
“Do you experience shortness of breath or a sensation of air hunger?”
“Are you experiencing any chest pain?”
Other causes of dizziness:
- Cerebrovascular disorders
Dizziness is a relatively common symptom of impaired blood flow to the brain, but it’s not the only one. Alongside dizziness, patients typically report numbness or weakness in one side of the body, difficulty understanding speech or speaking, double vision, unsteadiness while walking, loss of balance, or coordination problems. Patients with impaired cerebral circulation often have a medical history of hypertension, rhythm disturbances (such as atrial fibrillation), diabetes mellitus, and dyslipidemia. Neurological examination may reveal deficits such as hemiparesis or hemiplegia, sensory or motor aphasia, nystagmus, facial asymmetry, deviation of the tongue from the midline, inability to perform the thumb-nose test, instability in Romberg’s sign, among others. Blood pressure and heart rate typically remain normal or may show slight increases.
- Hypoglycemia
Patients experiencing hypoglycemia often report severe hunger, pronounced weakness, and increased sweating alongside dizziness. They typically have a history of taking hypoglycemic medications, prolonged fasting, or engaging in excessive physical activity. These patients may appear agitated, with cold, clammy skin, and the doctor may observe tachycardia and a moderate increase in blood pressure. The initial agitation can rapidly transition to central nervous system depression, leading to loss of consciousness.
- Arterial hypertension
Dizziness commonly accompanies high blood pressure. Additionally, patients with arterial hypertension often report a throbbing or aching headache, nausea, and visual disturbances like flickering. During the physical examination, the doctor typically observes elevated blood pressure readings ≥140/90 mm Hg and often notes tachycardia.
- Arterial hypotension
Dizziness can manifest as a symptom of both high and low blood pressure. Patients with hypotension also commonly experience pronounced weakness, lethargy, drowsiness, and reduced tolerance to physical exertion. These patients often have a history of taking vasodilators, diuretics, experiencing repeated vomiting, diarrhea, bleeding, or adhering to a diet with limited salt and water intake. During the physical examination, the doctor may observe pallor of the skin, increased sweating, cold extremities, and a decrease in blood pressure ≤90/60 mm Hg, accompanied by reduced urine output.
- Anemia
Dizziness is a common symptom of chronic anemia. Alongside dizziness, patients with anemia often report persistent pronounced weakness, increased fatigue, palpitations, shortness of breath, brittle nails and hair, pain in the tongue, and alterations in food preferences and taste. In their medical history, patients may mention dietary changes, avoidance of animal protein, gastrointestinal diseases, gastrointestinal surgeries, pregnancy, chronic hemorrhoidal bleeding, or prolonged menstruation. Physical examination typically reveals pallor of the skin and mucous membranes, tachycardia, a small, frequent pulse, and a functional systolic murmur.
- Meniere’s disease
Characteristic symptoms of Ménière’s disease include systemic dizziness, tinnitus, and progressive hearing loss. Typically, these symptoms occur in an episodic manner, often in the morning or at night, triggered by psychological or physical stressors. During an episode, patients may experience nausea, vomiting, and coordination disturbances. The duration of these episodes can range from a few minutes to several days, with the average being several hours.
Other reasons for episodes of loss of consciousness:
- Vasovagal syncope
Vasovagal syncope is a type of reflex syncope triggered by severe stress (such as fear, pain, the sight of blood, or medical procedures) or prolonged standing in an upright position. It typically develops gradually and is often preceded by symptoms like dizziness, visual disturbances, nausea, and increased sweating. During a vasovagal syncope episode, patients may experience involuntary movements, hypotension, and a decrease in heart rate. The duration of the episode usually does not exceed 1 minute, and patients typically regain consciousness spontaneously.
- Situational syncope
Situational syncope is another type of reflex syncope that occurs due to a sudden increase in intra-abdominal pressure, such as during a forceful cough, defecation, urination, or after eating a large meal. Similar to vasovagal syncope, situational syncope tends to develop gradually, with preceding symptoms like dizziness, nausea, and visual disturbances. During the episode, the patient may exhibit pallor, bradycardia, and hypotension. Situational syncope episodes typically last no more than 1 minute, and patients often regain consciousness spontaneously.
- Carotid sinus syndrome
Carotid sinus syndrome is characterized by hypersensitivity of the carotid sinus, often triggered by actions like a sharp turn of the head, wearing a tight collar, or shaving the neck. Before losing consciousness, patients may experience symptoms such as visual dimming and dizziness. During an episode of carotid syncope, marked pallor of the skin, along with a decrease in heart rate and blood pressure, is typically observed.
- Syncope due to orthostatic hypotension
Syncope due to orthostatic hypotension, on the other hand, occurs when there is a sudden drop in blood pressure upon moving from a horizontal to a vertical position. This type of syncope is commonly seen in the elderly and in individuals taking medications like diuretics, vasodilators, and antidepressants. Patients may also have hypovolemia due to conditions such as bleeding, repeated diarrhea, or vomiting. Diagnosis involves measuring blood pressure in both horizontal and vertical positions. A difference in systolic pressure of ≥20 mm Hg and/or diastolic pressure of ≥10 mm Hg upon changing positions suggests orthostatic hypotension. Unlike carotid sinus syndrome, patients with syncope due to orthostatic hypotension typically exhibit tachycardia rather than bradycardia.
- Syncope due to cerebrovascular disease
Syncope resulting from cerebral ischemia is typically accompanied by various neurological symptoms, including speech disorders, facial asymmetry, hemiparesis or hemiplegia, meningeal symptoms, ataxia, and others.
History of life
- Clarify whether the patient has previously been diagnosed with cardiovascular diseases, in particular myocardial infarction, angina pectoris, cardiomyopathy, congenital heart defects, myocarditis
- Find out if the patient has previously been diagnosed with a rhythm and/or conduction disorder
- Find out whether the patient suffers from infiltrative diseases, in particular sarcoidosis, hemochromatosis, amyloidosis; systemic diseases of connective tissue, such as rheumatoid arthritis, scleroderma, systemic lupus erythematosus; endocrine diseases, in particular hypothyroidism; neurological diseases accompanied by increased intracranial pressure
- Find out if the patient has had previous surgical interventions, including prosthetic heart valves, coronary artery bypass grafting, Maze procedure, and find out how the post-operative period was
- Find out if the patient is taking medications, including digoxin, beta-adrenergic blockers, calcium channel antagonists, antiarrhythmics, psychoactive drugs, clonidine, potassium, magnesium, calcium drugs; specify the doses of the drugs
- Find out if the patient has recently had an infectious disease and if the patient has been bitten by a tick
- Find out if the patient has a drug or food intolerance and how it manifests itself
- Find out if the patient has bad habits – drinking alcohol, drugs, smoking
- Determine whether the patient’s blood relatives have had cardiovascular disease, including rhythm and/or conduction disorders
- Find out the patient’s marital status, living conditions
- Clarify whether the patient works, his profession, working conditions, the presence of harmful occupational factors
Objective examination
- Assessment of the patient’s general condition
- Conducting a general inspection
- Evaluation of the constitution
- Estimation of the degree of obesity
- Skin and mucous membranes
- Evaluation of thyroid glands
- Assessment of peripheral lymph nodes
- Assessment of respiratory organs
- Evaluation of the cardiovascular system
- Assessment of abdominal organs
- Evaluation of organs of the genitourinary system
Assess for objects or equipment on or around the patient that may provide useful information about the patient’s medical history and current clinical condition.
The key, and sometimes the only, objective sign of symptomatic bradycardia is a slowing of the heart rate (HR) to less than 60 beats per minute.
In the case of a moderate decrease in heart rate, blood pressure remains normal, but with a significant decrease in heart rate, hypotension often occurs.
With a significant decrease in heart rate, acute heart failure may occur with the appearance of moist rales in the lungs, tachypnea, and cyanosis.
In the case of a disruption of the blood supply to the brain, a disturbance of consciousness is often observed.
Additionally, during the physical examination, it is important to pay attention to signs of a disease that has led to a decrease in heart rate.
Thus, additional III or IV heart sounds, gallop rhythm, systolic noise of mitral regurgitation, paradoxical splitting of the II sound, congestive rales in the lungs can suggest coronary heart disease.
In patients with myocarditis, weakening of the I heart tone, an additional III heart tone is often detected, and in those with congestion alongside myocarditis, an accent of the II tone is heard over the pulmonary artery, wet fine-vesicular rales, and swelling of the lower extremities.
In patients with restrictive cardiomyopathy, the systolic murmur of mitral regurgitation, weakening of the first heart sound, wet, small bubbling rales in the lungs, ascites, edema of the lower extremities, hepatomegaly, and swelling of the jugular veins can be detected in the late stages of the disease.
Endocarditis may be indicated by the detection during a physical examination of a characteristic skin shade similar to coffee with milk, systolic or diastolic regurgitation noise over the affected valve, Osler nodules (painful, red nodules on the fingers and toes), Janeway spots (painless hemorrhagic spots on the palms and soles), hepato- and splenomegaly.
In patients with sarcoidosis, skin changes such as erythema nodosum, papular or spot-papular rashes, small ulcers, generalized lymphadenopathy, moist rales in the lungs, hepatomegaly, and enlargement of the parotid salivary gland can be observed.
Bronze skin shade, ascites, swelling of the lower extremities, and signs of liver cirrhosis may indicate hemochromatosis.
Rheumatoid arthritis should be suspected in patients with signs of inflammation and deformation of the metacarpophalangeal and proximal interphalangeal joints.
Discoloration of the skin of the fingers and toes, thickening and atrophy of the skin, formation of radial wrinkles around the mouth, ulcers on the tips of the fingers, and telangiectasia may indicate scleroderma.
Dry skin, hair loss, hoarseness of voice, facial swelling, and hypotonia can indicate hypothyroidism.
Laboratory examination
- Blood analysis for electrolytes (required)
- Blood test for thyroid hormones and TSH (required)
- Clinical blood count (if needed)
- Coagulogram (if necessary)
- Blood test for creatinine and urea (if needed)
- Blood test for troponin- I (if necessary)
- Blood test for IgM and IgG antibodies to Borrelia (if necessary)
- PCR for Borrelia burgdorferi DNA detection (if necessary)
- Assessment of blood pH (if necessary)
- Genetic testing (if needed)
- Toxicological screening (if necessary)
- Blood test for electrolytes (required )
A blood test for potassium, calcium, and magnesium levels is a crucial laboratory assessment in patients presenting with symptomatic bradycardia to diagnose electrolyte imbalances. Hypokalemia, hyperkalemia, hypercalcemia, and hypermagnesemia are recognized causes of significant bradycardia.
- Blood test for thyroid hormones and TSH ( required )
A blood test for thyroid hormones and TSH is a crucial laboratory assessment in patients with symptomatic bradycardia, as hypothyroidism frequently manifests with a slow heart rate and conduction disturbances.
- Clinical blood test (if needed)
Clinical blood count is not typically considered mandatory for patients presenting with symptomatic bradycardia. However, it becomes necessary as part of pre-procedural preparations for pacemaker implantation.
- Coagulogram (if necessary)
A coagulogram is indeed included in the list of laboratory tests performed on patients with symptomatic bradycardia before a permanent cardiac pacing procedure to assess blood coagulation activity.
- Blood test for creatinine and urea (if needed)
Blood tests for creatinine and urea are indeed included in the list of laboratory tests performed in patients with symptomatic bradycardia before the procedure of permanent cardiac pacing.
- Blood test for troponin- I (if necessary)
A blood test for troponin-I is indeed performed in patients with symptomatic bradycardia when myocardial ischemia is suspected.
- Blood test for IgM and IgG antibodies to Borrelia (if necessary)
A blood test for IgM and IgG antibodies to Borrelia is indeed performed in patients with symptomatic bradycardia when Lyme disease is suspected.
- PCR for Borrelia burgdorferi DNA detection (if necessary)
Additionally, PCR for Borrelia burgdorferi DNA detection may be necessary in certain cases.
- Assessment of blood pH level (if necessary)
Assessment of blood pH level is also important in patients with symptomatic bradycardia, especially when metabolic acidosis is suspected, as it can contribute to bradycardia.
- Genetic testing (if needed)
Genetic testing for SCN5A and TRPM4 gene mutations may be needed in patients with symptomatic bradycardia, particularly when there is suspicion of a hereditary component to the rhythm or conduction disorder, especially in patients under the age of 50 who are experiencing symptoms.
- Toxicological screening (if necessary)
Toxicological screening is indeed indicated for suspected bradycardia induced by the action of a toxic substance or drug. For instance, when an overdose of cardiac glycosides is suspected, determining the level of digoxin in the blood is essential. Other tests aimed at detecting toxic substances in the body exist, but they typically require the involvement of a toxicologist.
Diagnostic tests
- Electrocardiography in 12 leads (required)
- Transthoracic echocardiography (mandatory)
- Ambulatory ECG monitoring (if necessary)
- ECG test with dosed exercise (if necessary)
- Coronary angiography (if necessary)
- MRI of the heart (if necessary)
- Positron emission tomography (if necessary)
- Electrophysiological examination (if necessary)
- Polysomnography (if necessary)
- Electrocardiography in 12 leads ( required )
Electrocardiography (ECG) in 12 leads is indeed a crucial method of examination for all patients with symptomatic bradycardia.
The primary causes of symptomatic bradycardia typically involve sinus node weakness syndrome and atrioventricular conduction disorders.
Manifestations of sinus node weakness syndrome encompass various abnormalities such as persistent sinus bradycardia, ectopic atrial bradycardia, sinoatrial block of different degrees, pacemaker migration, sinus node arrest with a pause lasting more than 3 seconds, bradysystolic form of atrial fibrillation, tachy-brady syndrome, and chronotropic incompetence.
ECG signs of persistent sinus bradycardia manifest as a sustained reduction in heart rate to less than 50 beats per minute.
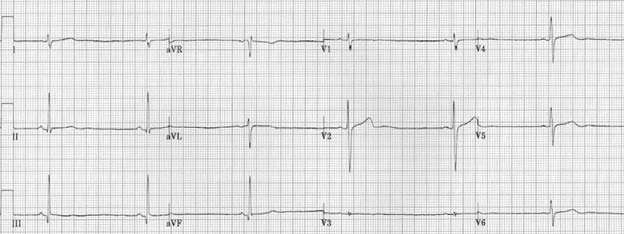
Figure 1. Atrial fibrillation. Image sourced from litfl.com internet resource. https://litfl.com/sinus-bradycardia-ecg-library
ECG signs of second-degree sinoauricular block include periodic loss of the PQRST complex, with the duration of the pause equal to the sum of two or more normal RR complexes of the underlying rhythm. During these pauses, substitute complexes originating from the AV node or ventricles may appear.
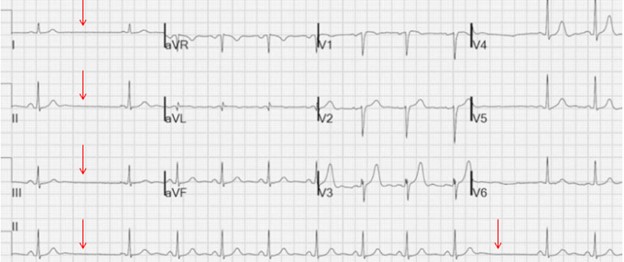
Figure 2. Second-degree sinoauricular block. Image sourced from litfl.com internet resource. https://litfl.com/sinoatrial-exit-block-ecg-library
ECG signs of complete sinoauricular block include the complete cessation of sinus rhythm with the appearance of a replacement rhythm, typically originating from the AV node.
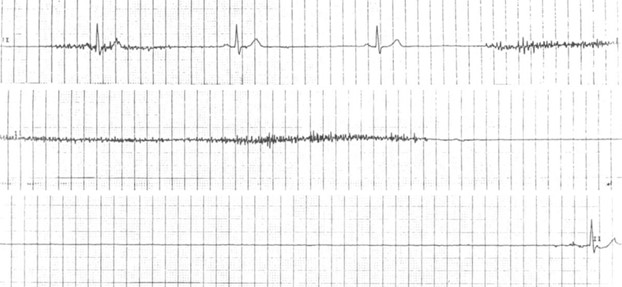
Figure 3. Complete sinoauricular block. Image from litfl.com internet resource. https://litfl.com/sinus-node-dysfunction-sick-sinus-syndrome
ECG signs of pacemaker migration include a gradual change in the shape and polarity of the P wave from cycle to cycle.
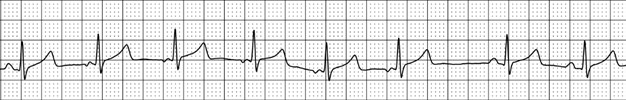
Figure 4. Migration of the pacemaker. Image https://therapy.odmu.edu.ua/ecg-online-course/wandering-pacemaker
ECG signs of tachy-brady syndrome include alternating episodes of acceleration and deceleration of the heart rate.
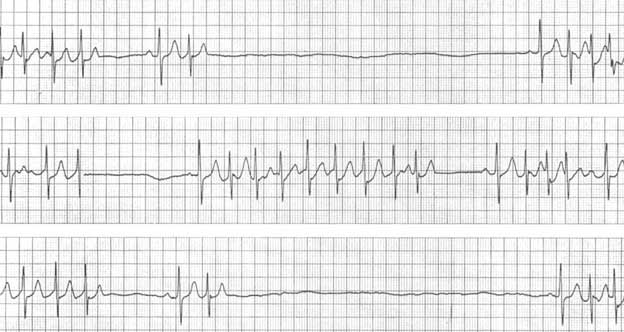
Figure 5. Tachy-brady syndrome. Image from litfl.com internet resource. https://litfl.com/sinus-node-dysfunction-sick-sinus-syndrome
ECG signs of Mobitz I second-degree AV block include progressive lengthening of the PQ interval with periodic loss of QRS complexes.
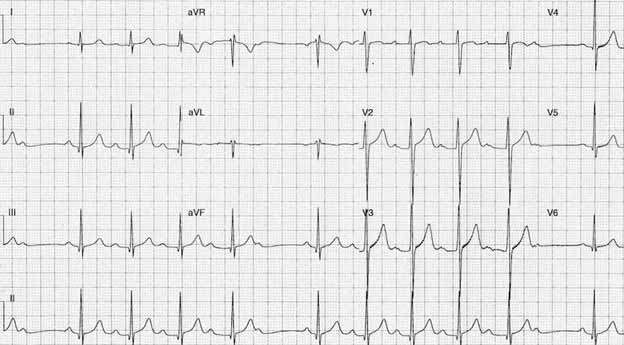
Figure 6. Second-degree AV block II, Mobitz I. Image from the internet resource litfl.com. https://litfl.com/av-block-2nd-degree-mobitz-i-wenckebach-phenomenon
ECG signs of Mobitz II second-degree AV block include stable prolongation of the PQ interval with periodic loss of QRS complexes.
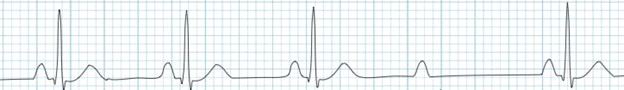
Figure 7. Second-degree AV-block, Mobitz II. Image from litfl.com internet resource. https://litfl.com/av-block-2nd-degree-mobitz-ii
ECG signs of third-degree AV block include complete dissociation of atrial and ventricular waves, with the atrial contraction frequency significantly exceeding the frequency of ventricular activation.
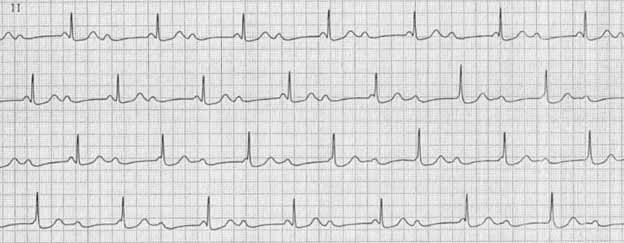
Figure 8. Third-degree AV block. Image from litfl.com internet resource. https://litfl.com/av-block-3rd-degree-complete-heart-block
- Transthoracic echocardiography (mandatory)
Transthoracic echocardiography is a crucial examination method for all patients presenting with symptomatic bradycardia. It aids in identifying myocardial structural abnormalities that could contribute to heart rate slowing, assessing left ventricular systolic function, and diagnosing potentially reversible causes of cardiac conduction disturbances.
- Ambulatory ECG monitoring (if necessary)
Ambulatory ECG monitoring is recommended when there’s a need to confirm the direct relationship between ECG changes and clinical manifestations.
- ECG test with dosed exercise (if necessary)
An ECG test with dosed exercise is conducted for patients who develop bradycardia during or immediately after physical activity. If symptoms arise during exercise, it may suggest a cardiac cause, while post-exercise bradycardia could indicate a reflex mechanism.
- Coronary angiography (if necessary)
Coronary angiography is indicated for patients with suspected ischemic causes of bradycardia or those with a significant family history.
- MRI of the heart (if necessary)
MRI of the heart is performed to investigate suspected inflammatory or infiltrative heart diseases contributing to bradycardia.
- Positron emission tomography (if necessary)
Positron emission tomography aids in complex cases by detecting myocardial inflammation foci.
- Electrophysiological examination (if necessary)
Electrophysiological examination serves as an adjunct when non-invasive methods fail to record bradycardia. It’s particularly useful for identifying sinus node dysfunction or pinpointing the site of impaired AV conduction.
- Polysomnography (if necessary)
Polysomnography is conducted for patients experiencing nocturnal bradycardia episodes, often associated with obstructive sleep apnea syndrome.
Differential diagnosis
Diagnosing symptomatic bradycardia typically isn’t challenging, but determining its cause can be more complex.
Common causes include acute myocardial ischemia, overdose of medications like cardiac glycosides, beta-blockers, and calcium channel antagonists, hyperkalemia, hypothermia, and hypoxia.
Acute myocardial ischemia presents with chest pain radiating to the left arm, scapula, or epigastrium. Elevated myocardial necrosis markers (troponin-I/T, CK-MB), along with characteristic ECG changes (ST segment elevation/depression, pathological Q wave, T wave inversion), are observed. Heart conduction issues often accompany ischemia affecting the lower left ventricular wall, considering the shared vascular supply.
Glycoside intoxication manifests as dyspeptic symptoms (anorexia, nausea, vomiting, diarrhea), visual disturbances (yellowish perception), and pulse slowing to asystole. ECG findings include ventricular extrasystoles, PQ interval prolongation, pacemaker migration, and trough-like ST segment depression. Suspected cases warrant digoxin-level assessment.
Beta-adrenergic blockers or calcium channel antagonist overdose leads to sinus and AV node depression with a substitute rhythm. Symptoms range from mild fatigue to dizziness and syncope. Detailed history-taking aids in diagnosis.
Hyperkalemia occurs in severe renal impairment, ACE inhibitor/sartan use, potassium supplements, aldosterone receptor blockers, rhabdomyolysis, metabolic acidosis, and sepsis. Diagnosis involves serum potassium assessment, and ECG may show high-amplitude T waves and intraventricular conduction abnormalities.
Hypothermia-induced bradycardia arises from prolonged cold exposure, typically exhibiting Osborne waves on the ECG.
Hypoxia, with blood oxygen saturation below 95%, presents with headache, dizziness, pallor, rapid breathing, and impaired memory and attention. Pulse oximetry is the primary diagnostic tool. Identifying the underlying cause of hypoxia – cardiovascular or respiratory diseases, anemia, vasculitis, altitude exposure, suffocation, drowning – is crucial. The effectiveness of oxygen therapy in restoring normal heart rhythm confirms the link between hypoxia and AV conduction slowing.
Making a clinical diagnosis
- Identification of the underlying disease
- Indication of the nature of the conduction disturbance that caused the bradycardia
- Indication of comorbid pathology
- Identification of the underlying disease
Given that bradycardia is typically a manifestation or complication of an underlying disease, it’s crucial to first specify the primary diagnosis and then the associated rhythm disturbance. This approach aligns with existing classifications and ensures clarity in diagnosis.
- Indication of the nature of the conduction disturbance that caused the bradycardia
When identifying the conduction disturbance causing bradycardia, denote its type and degree: first-, second-, or third-degree sinoauricular block or atrioventricular block.
- Indication of comorbid pathology
In formulating the clinical diagnosis, specify any comorbid conditions according to established classifications.
Specialist consultations
- Cardiologist
- Cardiac surgeon
- Arithmologist
- Rheumatologist
- Neuropathologist _
- Endocrinologist
- Nephrologist
- Geneticist
- Infectious Disease Specialist
A cardiologist serves as the primary specialist overseeing the management of bradycardia. They lead the diagnostic and treatment process, conducting thorough examinations, taking medical histories, prescribing treatment protocols, monitoring patient progress, and making necessary adjustments.
- Cardiac surgeon
Consultation with a cardiac surgeon becomes necessary when bradycardia is suspected to be induced by myocardial ischemia or a heart defect. The cardiac surgeon performs surgical corrections for these conditions, which can help alleviate bradycardia.
- Arithmologist
Given that pathological heart rate slowing often stems from sinus node weakness syndrome or AV conduction disturbances, an arrhythmologist’s assistance is invaluable. They determine the nature of existing rhythm or conduction disorders, including through electrophysiological studies, and if required, perform pacemaker implantation.
- Rheumatologist
If collagenosis is suspected as the cause of bradycardia, consulting a rheumatologist is necessary. Through additional laboratory or instrumental examinations, this specialist can confirm or rule out autoimmune connective tissue pathology.
- Neurologist
A neurologist’s consultation is necessary if a neurogenic cause of bradycardia is suspected, particularly due to central nervous system injuries or tumors leading to increased intracranial pressure. Additionally, since symptomatic bradycardia often coincides with alterations in mental status, a neurologist aids in differential diagnosis, especially against acute cerebral circulation disruptions.
- Endocrinologist
If hypothyroidism is suspected as the cause of symptomatic bradycardia, consultation with an endocrinologist is warranted.
- Nephrologist
Hyperkalemia is a common cause of slow heart rate, particularly in patients with severe renal impairment, necessitating consultation with a nephrologist.
- Geneticist
When hereditary conduction system disorders are suspected, especially if symptoms manifest before the age of 50 and progress over time, genetic consultation is essential.
- Infectious Disease Specialist
Consultation with an infectious disease specialist is advisable if an infectious disease is suspected as the cause of symptomatic bradycardia, such as Lyme disease or diphtheria.
Treatment
- Emergency therapy
- Long-term therapy (permanent cardiac stimulation)
- Emergency therapy
When administering emergency care to a patient with symptomatic bradycardia, it’s crucial to adhere to the following algorithm of actions:
- Ensure the patency of the respiratory tract.
- Initiate oxygen therapy for hypoxemia (blood oxygen saturation <90%).
- Monitor heart rate and blood pressure.
- Establish intravenous access.
- Consider potential causes of symptomatic bradycardia (discontinue drugs and, if possible, administer their antidotes; perform myocardial revascularization in acute ischemia; correct hyperkalemia).
In case of the development of hypotension, impaired consciousness, symptoms of acute heart failure, or myocardial ischemia, medical treatment is indicated:
- Administer atropine in a dose of 0.5-1.0 mg IV, with the possibility of repeated administration every 3-5 minutes if necessary (maximum dose – 3 mg).
- If atropine is ineffective, consider using dopamine at a dose of 5-20 μg/kg/min. or epinephrine at a dose of 0.02-0.2 μg/kg/min. IV drip.
If drug treatment proves ineffective, electrocardiostimulation is indicated, with preference given to temporary transvenous cardiostimulation. If transvenous cardiostimulation is not feasible, transcutaneous cardiostimulation may be considered.
It’s worth noting that administering aminophylline in a dose of 250 mg IV as a bolus is recommended for patients with second or third-degree AV block occurring against the backdrop of an acute lower myocardial infarction.
In cases of overdose with calcium channel antagonists, consider administering a 10% solution of calcium chloride in a dose of 1-2 g every 10-20 minutes intravenously or as an intravenous infusion at a rate of 0.2-0.4 ml/kg/h; alternatively, a 10% solution of calcium gluconate can be given in a dose of 3-6 g every 10-20 minutes intravenously or as an intravenous infusion at a rate of 0.6-1.2 ml/kg/h.
For beta-adrenergic blocker overdose, glucagon may be used at a dose of 3-10 mg IV as an infusion at a rate of 3-5 mg/h.
In cases of digoxin overdose, consider administering digibind at a rate of 1 vial to bind 0.5 mg of digoxin in the blood.
Patients with a transplanted heart or those with sinus node weakness syndrome due to spinal cord injury may benefit from aminophylline at a dose of 6 mg/kg, dissolved in 100-200 ml of physiological solution IV drip over 20-30 minutes, or theophylline 300 mg IV followed by oral administration at a dose of 5-10 mg/kg.
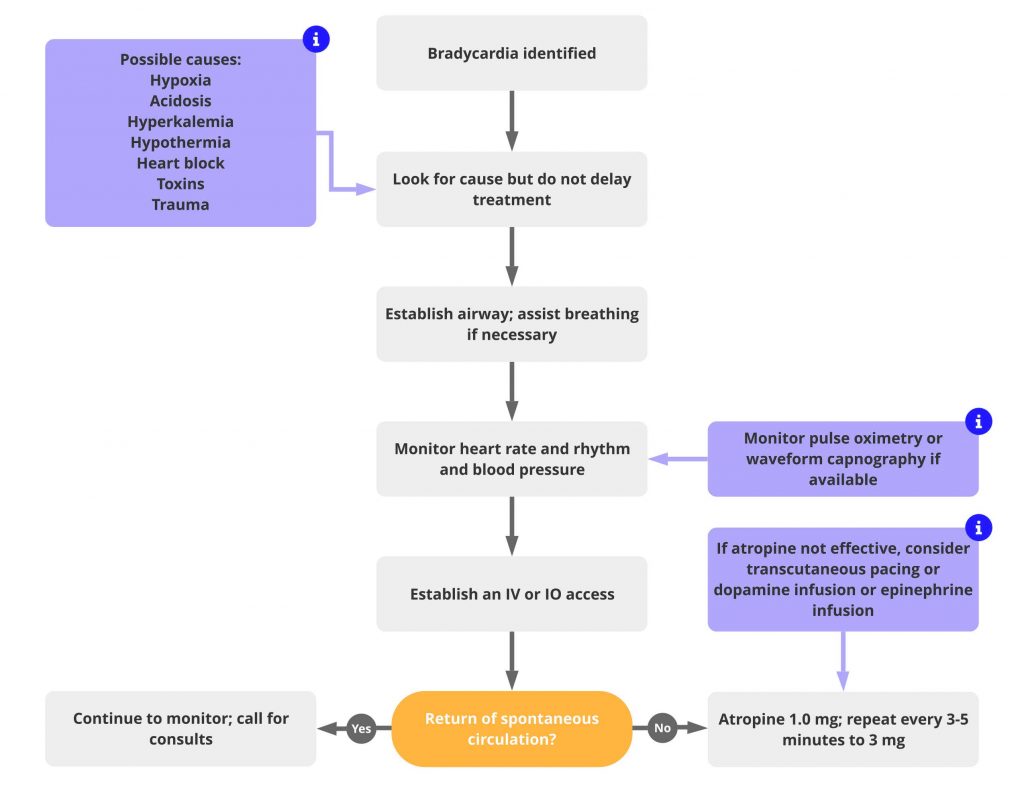
ACLS Bradycardia Algorithm
- Long-term therapy (permanent cardiac stimulation)
The choice of long-term therapy for patients with sinus node weakness syndrome depends on the presence of bradycardia symptoms:
- Observation is indicated for asymptomatic patients with sinus bradycardia or sinus pauses caused by sinus node syndrome, vagotonia, or nocturnal sleep apnea syndrome. Continuous cardiac stimulation may cause more harm than good in these cases.
- Symptomatic patients with bradycardia caused by sinus node syndrome are indicated for continuous pacing to increase heart rate and improve symptoms.
The choice of cardiac stimulation type depends on the frequency of necessary stimulation and the presence of concomitant pathology:
- For infrequent stimulation or in the presence of severe concomitant pathology, single-chamber ventricular cardiostimulation is advisable.
- If frequent stimulation is necessary, and there is no severe concomitant pathology with normal AV conduction, single-chamber atrial cardiostimulation is recommended.
- If frequent stimulation is necessary without severe concomitant pathology but with impaired AV conduction, two-chamber cardiostimulation is recommended.
Long-term therapy for patients with AV conduction disorders depends on the severity of the blockade and bradycardia symptoms:
- Asymptomatic patients with first-degree AV block or Mobitz type I second-degree AV block are observed; continuous cardiac stimulation may not be beneficial.
- Symptomatic patients with first-degree AV block or Mobitz type I second-degree AV block may consider permanent pacing.
- Symptomatic patients with Mobitz type II second-degree AV block and third-degree AV block are recommended for permanent cardiac stimulation.
The choice of cardiac stimulation type depends on the required frequency of stimulation and concomitant pathology:
- For infrequent stimulation or severe concomitant pathology, single-chamber ventricular cardiostimulation is advisable.
- For frequent stimulation without severe concomitant pathology, single-chamber ventricular cardiostimulation is recommended, especially for patients with a permanent form of atrial fibrillation.
- For frequent stimulation without severe concomitant pathology and without a permanent form of atrial fibrillation, two-chamber cardiostimulation is recommended.
Explain the procedure for cardiac stimulation
- Check the patient’s understanding of the reason for the procedure
- “Do you understand the reason for performing this procedure on you?”
- “Do you understand the importance of carrying out this procedure for you?”
- Check the patient’s understanding of the procedure
“Did you understand the procedure?”
- Inform about the stages of the procedure
“I would like to explain to you what electrical cardiostimulation is and how it is performed. Electrical cardiac stimulation is a medical procedure aimed at normalizing the heart rhythm. Before conducting electrical cardiostimulation, you will be given a sedative and painkiller so that you feel comfortable and do not have any unpleasant sensations. After that, the surgeon will make a small skin incision under your collarbone and insert a special electrode into the subclavian vein. Under X-ray control, the doctor will lead this electrode to your heart and fix it in the right place. Then the surgeon will make a small pocket under your skin on the chest where a special pacemaker device will be located. This device will generate electrical impulses that will be conducted through the electrode to your heart. Thanks to this, your heart will contract in the correct rhythm. During the entire procedure and for some time after it, an experienced medical staff will be by your side, who will carefully monitor your condition.”
- Talk about the risks and complications
“This procedure is quite safe, but sometimes patients may experience complications, for example, hematoma in the area of the formed subcutaneous pocket, infection, or displacement of the electrode. However, we will do everything possible to minimize the risk of their development.”
- Do the work of mitigating fears
- “This procedure is routine for our clinic.”
- “This procedure is constantly performed in our department.”
- Suggest an additional source of information
“You can learn more about the cardiac pacing procedure by reading the information in this booklet“
Consulting and support
- Inform the patient about the disease
- Explain to the patient the possible causes of the disease
- Inform the patient of the symptoms that may occur with the identified disease
- Discuss the results of the examinations with the patient
- Explain to the patient the possible consequences of the disease
- Educate the patient about available treatments
- Help the patient understand the risks and benefits of different treatments
- Answer the patient’s questions
- Provide an explanation of the extent of monitoring during and after treatment
- Schedule regular check-ups and follow-up to assess the effectiveness of treatment and changes in the patient’s condition
| Inform the patient about the disease | “Mr./Ms. [Last Name], I would like to inform you of your diagnosis. You have a significant slowing of the heart rate, known as bradycardia. Bradycardia results from a malfunction of the heart’s conduction system, such as sinus node weakness syndrome or atrioventricular block. With sinus node weakness syndrome, the generation or conduction of electrical impulses to the atria is disrupted, leading to a slower heart rate. With atrioventricular block, electrical impulses are generated normally but may be significantly delayed or completely blocked from reaching the ventricles. Due to inadequate oxygen and nutrient supply, all organs and systems suffer, particularly the brain and heart.” |
| Explain to the patient the possible causes of the disease | “There are various reasons for conduction system disorders of the heart, categorized as internal (cardiac) or external (extracardiac). Common causes include myocardial ischemia, elevated blood potassium levels, certain medications, or central nervous system damage. Less frequent causes include hypothermia, hypothyroidism, myocardial inflammation, and sleep apnea syndrome. Additional examinations will be needed to pinpoint the specific cause of your bradycardia, enabling us to determine the most effective treatment.” |
| Inform the patient of the symptoms that may occur with the identified disease | “Bradycardia may often be asymptomatic, but significant slowing of the heart rate can lead to noticeable complaints. Mild cases may cause feelings of fatigue, weakness, or reduced tolerance to physical exertion. Severe cases can result in shortness of breath, chest pain, or even loss of consciousness due to impaired blood supply to the heart and brain.” |
| Discuss the results of the examinations with the patient | “Mr./Ms. [Last Name], I want to share the results of your examinations with you. Electrocardiography revealed a significant slowing of the heart rate, stemming from impaired electrical impulse conduction through the heart. Blood tests showed normal laboratory parameters. To assess your heart’s blood supply, we conducted a coronary angiography, which revealed minor cholesterol deposits in your blood vessels, but they do not significantly affect blood flow to the heart. Do you have any questions about the information I’ve provided?” |
| Explain to the patient the possible consequences of the disease | “The severity of the consequences of bradycardia depends on the heart rate. Heart rates above 50 beats per minute typically do not result in negative consequences. However, heart rates below 50 beats per minute may lead to decreased blood pressure, altered consciousness, and heart ischemia, which pose significant health risks.” |
| Educate the patient about available treatments | “I’d like to discuss the treatment options for bradycardia. If your bradycardia is asymptomatic or mildly symptomatic, observation may suffice without intervention. However, in cases of life-threatening symptoms like loss of consciousness or chest pain, treatment is necessary. Initial treatment often involves atropine to improve electrical impulse conduction in the heart. If atropine is ineffective, other medications like epinephrine or dopamine may be used. Electrical cardiostimulation is commonly employed if medications are ineffective. If bradycardia is due to a reversible cause, temporary transcutaneous cardiostimulation may be sufficient until normal heart rhythm is restored. For irreversible cases, permanent pacemaker implantation is recommended. A pacemaker generates electrical impulses, ensuring the heart beats at the correct rate.” |
| Help the patient understand the risks and benefits of different treatments | “Although electrical cardiostimulation is generally safe when performed by experienced medical professionals, there is a small risk of complications such as infection or bleeding at the electrode insertion site, perforation of the heart, or electrode displacement. However, we will take all necessary precautions to minimize these risks.” |
| Answer the patient’s questions | “If you have any questions about the causes, symptoms, diagnosis, or treatment of your condition, please don’t hesitate to ask. It’s essential that you understand your condition and the next steps in your care.” |
| Provide an explanation of the extent of monitoring during and after treatment | “Monitoring your condition is crucial for timely assessment and correction of any changes and evaluating treatment effectiveness. We will monitor your general condition, blood oxygen saturation, blood pressure, and heart rate. Pulse oximetry will assess blood oxygen saturation, while blood pressure monitoring helps evaluate heart function. Electrocardiography will monitor heart rhythm. Regular follow-ups with your family doctor and arrhythmologist are essential for ongoing monitoring and pacemaker assessment.” |
| Schedule regular check-ups and follow-up to assess the effectiveness of treatment and changes in the patient’s condition | “After discharge, it’s important to monitor your well-being. Keep a diary noting any changes in symptoms, pulse, or blood pressure. Regular visits to your family doctor for electrocardiogram monitoring and arrhythmologist appointments, initially every 4-6 weeks and later every 6-12 months, are recommended. Modern pacemakers may include remote monitoring systems, enabling your doctor to assess pacemaker function remotely and detect any issues.” |
Monitoring the effectiveness of treatment
- Clinical assessment
The effectiveness of treatment is clinically assessed by evaluating both subjective symptoms reported by the patient and objective parameters of the body’s functioning. Effective treatment should alleviate or significantly reduce symptoms associated with insufficient organ and system blood supply due to bradycardia. These symptoms may include fatigue, decreased tolerance to physical activity, dizziness, fainting, chest discomfort, and shortness of breath.
- Studies to assess the presence of bradycardia
Objective assessment of bradycardia severity requires regular electrocardiography and, if necessary, daily Holter ECG monitoring. These tests provide valuable information about heart rhythm patterns and any fluctuations in heart rate over time.
- Control over side effects of therapy
Following pacemaker implantation, patients should be monitored for potential side effects or complications. Common complications include discomfort or pain at the implantation site, hematoma formation, infection at the pacemaker site, systemic infection, allergic reactions to pacemaker materials, and impaired wound healing. Patients should be educated about these potential side effects and instructed to seek immediate medical attention if they experience any symptoms suggestive of these complications. Early detection and intervention are crucial for managing complications effectively.
End of consultation
- Summarize the data and ask the patient if anything important has been missed
- Inform the patient about further tactics
Hospitalization in a specialized cardiology hospital is recommended for a comprehensive examination and the selection of optimal treatment strategies. Ensure the patient’s Informed Voluntary Consent for diagnosis and treatment and obtain agreement for processing personal data.
- Thank the patient
- Dispose of PPE properly and wash hands
Key communication skills
- Active listening
- Summing up
- Selection of indicative signs

Responses