Clinical Presentation Alzheimer Disease

Clinical case Alzheimer disease
- 1. Discuss the differential diagnoses of dementia
- 2. Identify the clinical manifestations of Alzheimer disease
- 3. Discuss the diagnosis of Alzheimer disease
- 4. Describe the pathologic features of Alzheimer disease
- 5. Review the mechanism of action of drugs used in the management of Alzheimer disease
- Cognitive decline in the setting of cerebrovascular disease
- Second leading cause of dementia
- Suspected in the presence of long-standing hypertension or diabetes mellitus
- Multiple small cerebral infarcts can result in the loss of cognitive function
- CT and MRI show previous cerebral infarcts
- Focal atrophy of the frontal and temporal lobes on brain CT or MRI
- Deposition of tau protein in the brain (Pick bodies)
- Most commonly affects males over 60 years old
- Language and behavior become abnormal first
- Memory is preserved until later stages
- Dementia in the presence of parkinsonian signs:
- Resting tremor
- Shuffling gait
- Fluctuations in cognitive function with periods of alertness and attention
- Visual hallucinations in more than 75% of cases
- Autosomal dominant degenerative disorder of adult onset
- Movement disorders, neuropsychiatriс manifestations, and dementia
- A spongiform encephalopathy
- Rapidly progressive dementia following infection with prion proteins
- Most commonly affects elderly males
- Clinical triad:
- Dementia
- Gait disturbances
- Urinary incontinence = “Wacky, Wobbly and Wet”
- CT and MRI show enlarged cerebral ventricles
- Neurodegenerative disorder of unknown cause
- Primarily presents in patients over 65 years of age
- Most common cause of dementia (70% of cases)
- First clinical manifestation is memory impairment in the form of anterograde episodic amnesia
- Characteristic pattern of memory impairment:
- Early loss of recent memory (hippocampus)
- Immediate, distant, and procedural memory are preserved until later stages of disease
- Other forms of cognitive impairment:
- Language and visuospatial skills are affected first
- Behavioral and executive dysfunction appear later
- Apraxia manifests as the inability to perform learned motor tasks
- Poor judgment, poor planning, or poor insight
- Anosognosia, or loss of insight into one’s own disorder, is characteristic of Alzheimer disease
- Patients trivialize severity of their condition
- Neuropsychiatrie manifestations:
- Changes in personality
- Aggression
- Agitation
- Psychosis
- 30% of patients suffer from depression
- Focal neurologic deficits may appear
- There is no diagnostic test for Alzheimer disease
- Diagnosis must be made clinically once all other causes of dementia have been excluded
- Exclusion tests include:
- Complete blood count
- Electrolyte panel
- Levels of thyroid hormone, liver enzymes, vitamin B-12
- RPR (rapid plasma reagin) is a screening test for syphilis
- HIV ELISA
- Brain CT, MRI
- Usually confirmed postmortem, following autopsy and histopathologic examination of the patient’s brain tissue
- The pathogenesis of Alzheimer disease is unknown
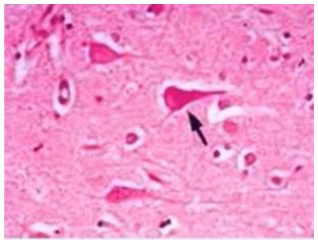
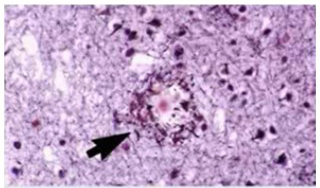
- Microscopic findings characteristic of Alzheimer disease are not pathognomonic for it:
- Neurofibrillary tangles
- Senile plaques
- Granulovacuolar degeneration
- Amyloid angiopathy of small to medium-sized brain vessels
- Macroscopic findings:
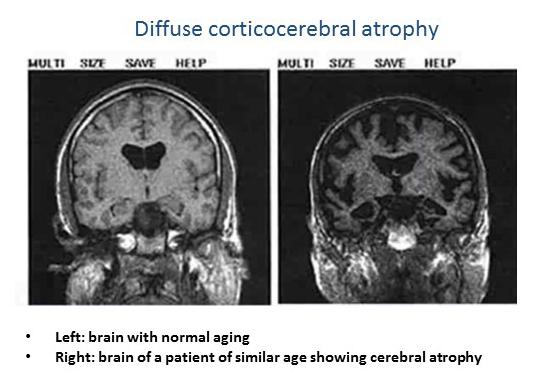
- Diffuse cerebral and/or cortical atrophy
- Hippocampal atrophy
- Made of phosphoryiated tau protein:
- A stabilizer of microtubules found in neurons
- When phosphoryiated, forms insoluble intraneuronal inclusions:
- Interfere with proper functioning
- Lead to neuronal degeneration
- Most prominent in the hippocampal region
- Neurofibrillary tangle count strongly correlates with disease severity
- Composed of beta-amyloid deposits in the extracellular brain matter
- A small number of plaques can be a physiologic finding as a result of the normal aging process
- A large number of plaques is consistent with Alzheimer disease
- Mutations in certain genes could be responsible for the increased deposition of amyloid protein:
- Amyloid precursor protein (APP) gene (chromosome 21)
- Presenilin 1 gene (chromosome 14)
- Presenilin 2 gene (chromosome 1)
- The role of chromosome 21 in the production of amyloid precursor protein has been speculated to contribute to the high prevalence of Alzheimer disease in people with trisomy 21
- Down syndrome patients are known to develop Alzheimer disease in their forties, 15-20 years before the general population
- Cholinestrase inhibitors (donepezil) are indirect-acting cholinomimetics:
- Prevent the breakdown of acetylcholine in the synaptic cleft
- Acetylcholine is a neurotransmitter involved in synaptic plasticity:
- Allows for synapses to change, thereby allowing for learning and memory
- Patients have a marked reduction in the activity of choline acetyltransferase in the cerebral cortex and hippocampus
- By increasing the amount of acetylcholine available in neural junctions, cholinesterase inhibitors are thought to slow the progression of neuronal degeneration
- The N-methyl-D-aspartate (NMDA) receptor:
- Involved in learning and memory
- Found abundantly within hippocampal and cortical neurons
- Glutamate:
- The main excitatory neurotransmitter acting on these neurons
- Activates the NMDA receptor by increasing the flow of cations through non-selective channels
- Excessive stimulation of the NMDA receptor by glutamate can result in neurotoxicity
- Memantine:
- Thought to block excessive activity of the NMDA receptor while preserving its normal functions (neuroprotective effect)
- Used in combination with cholinesterase inhibitors
- Antidepressants, valproic acid, and other mood stabilizers can also prove useful in the treatment of Alzheimer disease
Learning Objectives:
Dementia – the loss of cognitive ability severe enough to represent a decline from a previous level of functioning.
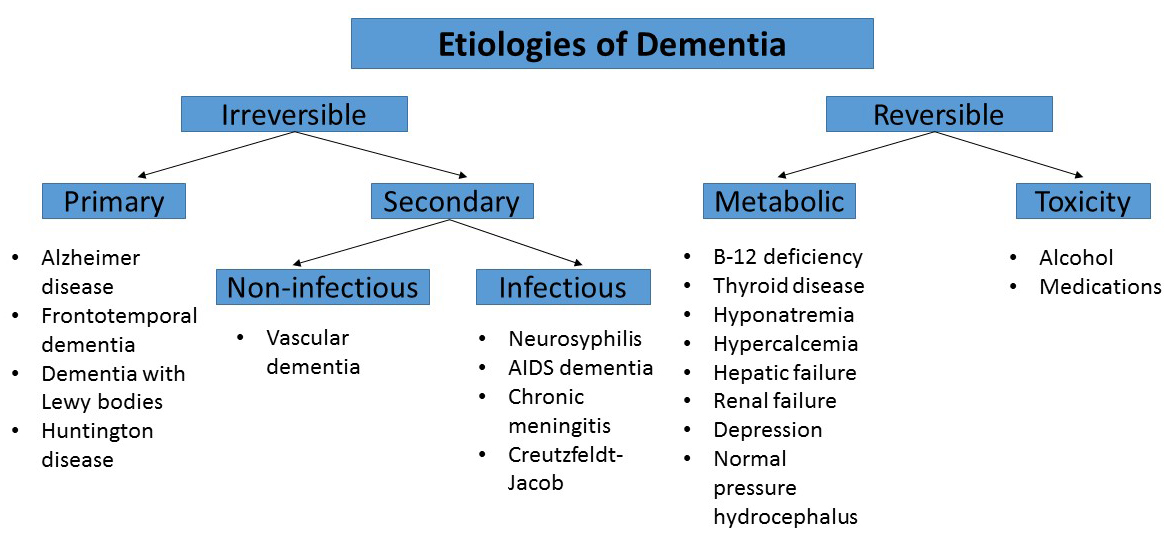
1. Differential diagnoses of dementia
Vascular Dementia
Frontotemporal Dementia (Pick Disease)
Lewy Body Dementia
Huntington Disease
Creutzfeldt-Jakob Disease
Other causes of dementia are those known as reversible causes these can be related to alcohol and medication intake or metabolic disorders such as vitamin B-12 deficiency, thyroid disease, hyponatremia, hypercalcemia and hepatic and renal dysfunction.
Detection and subsequent correction of these conditions may lead to reversal of dementia symptoms making their early diagnosis critically important another cause of reversible dementia is normal pressure hydrocephalus.
Normal Pressure Hydrocephalus
Alzheimer Disease
2. Clinical manifestations of Alzheimer disease
Memory Impairment
Executive Dysfunction
Later Stages
3. Diagnosis of Alzheimer disease
4. Pathologic features of Alzheimer disease
Neurofibrillary Tangles
Senile Plaques
Alzheimer Disease in Down Syndrome
5. Treatment of Alzheimer disease
No cure for Alzheimer disease, but early treatment has been shown to slow progression.
Cholinesterase Inhibitors
NMDA Receptor Antagonist (Memantine)
Mood Stabilizers
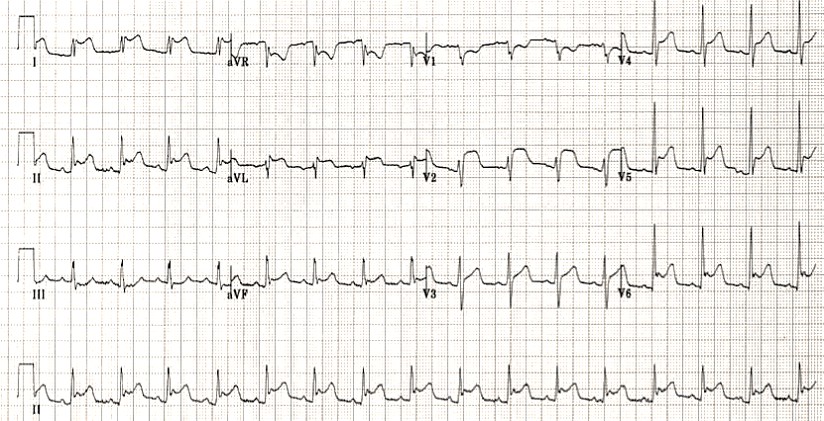
CT or MRI in patients with Alzheimer disease
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Celebrating a Major Milestone: SESAM Recognizes ClinCaseQuest’s Defragmented Debriefing Model as an Advancement in Clinical Simulation 2024
At ClinCaseQuest, we are thrilled to announce an outstanding achievement in the field of medical…
Acute Pulmonary Edema: Emergency Care Algorithm – Should We Remove or Redistribute the Fluid?
Case Presentation: A 64-year-old man was transported to the emergency department by ambulance due to…
ClinCaseQuest Featured in SchoolAndCollegeListings Directory
Exciting News Alert! We are thrilled to announce that ClinCaseQuest has been successfully added to…
Сounseling a patient with suspected Takotsubo-syndrome OSCE guides
The onset of the consultation Wash hands and put on PPE if necessary. Introduce yourself…
Takotsubo syndrome
Takotsubo syndrome is a condition characterized by the sudden onset of acute, transient (lasting up…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…