Patient’s counseling with an increased INR level / OSCE guide

- Opening the consultation
- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role
- Confirm the patient’s name and date of birth
- Explain the reason for the consultation
- Ideas, concerns, complications and expectations
- Explore what the patient currently understands about increased INR
- Ask if the patient has any concerns about warfarin
- Ask if the patient is bleeding now or before counseling
- Explore what the patient is hoping to get out of the consultation
- Analysis of earlier, current INR results, apropriate INR target range and current warfarin dosing
- Evaluate previous warfarin dosages
- Evaluate the patient’s earlier INR results
- Assess the patient’s apropriate INR target range
- Evaluate the results of the current INR
- Analysis of the factors that may affect the increased INR level
- Assess the presence of warfarin taking errors, low patient compliance, the complexity of the warfarin regimen for the patient
- Assess any changes in the patient’s clinical condition
- Evaluate any changes in medication
- Evaluate any changes in lifestyle
- Evaluate changes in alcohol consumption
- Providing medical care to the patient if necessary
- Assess the patient’s bleeding and its severity if necessary
- In case of active bleeding, provide immediate medical care after taking INR results
- In the absence of bleeding adjust the dosage of warfarin
- Assess the patient’s bleeding and its severity if necessary
- Bleeding whilst taking warfarin
- Explain that the main side effect of warfarin is bleeding more easily than normal
- Explain the common types of ‘less serious bleeding’ and what to do if they experience them
- Explain the rarer types of ‘serious bleeding’ and what to do if they experience them
- How to take warfarin
- Explain that warfarin should be taken at the same time each day
- Explain the different types of warfarin tablets
- Explain what the patient should do if they forget a dose
- Advise the patient to let medical professionals know that they take warfarin when they are being prescribed new medications
- Advise the patient to let the team managing their anticoagulation know when they start taking a new medication
- Advise the patient about the importance of effective contraception if taking warfarin (if relevant)
- Tips for further warfarin dosing according to the analysis of the reasons that led to the INR levels increase
- Estimate the required duration of administration of a concomitant drug that interacts with warfarin (temporary, chronic) as needed
- Adjust warfarin dosage as needed
- Withdraw warfarin if necessary
- Evaluate the rationality and necessity of co-administration of antiplatelet agents and nonsteroidal anti-inflammatory drugs if necessary
- Lifestyle advice
- Advise the patient about the impact of diet on the effect of warfarin
- Advise the patient about the impact of alcohol on the effect of warfarin
- Advise the patient about brushing teeth, shaving and dental procedures
- Yellow booklets and alert card
- Provide the patient with information about the INR monitoring booklet and patient information booklet
- Explain the importance of carrying the anticoagulant alert card with them at all times
- Closing the consultation
- Summarise the key points back to the patient
- Ask the patient if they have any questions or concerns that have not been addressed
- Arrange appropriate follow-up
- Thank the patient for their time
- Dispose of PPE appropriately and wash your hands
- Key communication skills
- Active listening
- Summarising
- Signposting
- Key clinical skills
- Determining the target INR level depending on the clinical situation
- Analysis of the factors that may affect the INR increase
- Providing medical care to the patient with INR increase
- Advice to the patient and explanations about lifestyle, diet
Opening the consultation
- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role.
- Confirm the patient’s name and date of birth
- Explain the reason for the consultation
Ideas, concerns, complications and expectations
- Explore what the patient currently understands about increased INR
- Ask if the patient has any concerns about warfarin
- Ask if the patient is bleeding now or before counseling
- Explore what the patient is hoping to get out of the consultation
| Ideas | Explore what the patient currently understands about increased INR | “Have you heard of increased INR?” “Do you understand the reasons that can cause an INR increase?” “Have you ever had an INR increase before? What did cause it early?” |
| Concerns | Ask if the patient has any concerns about warfarin | “Is there anything that worries you about taking warfarin?” |
| Complications | Ask if the patient is bleeding now or before counseling | “Are you bleeding at this moment, or before counseling?” “Have you had periods that are more intense and last longer than usual?” “Have you had bleeding that stops for a little longer than usual? “Have you had a nosebleed (lasting more than 10 minutes)?” “Did you have bleeds from your gums while brushing your teeth?” “Have you had bruises that appear for no reason?” “Did you have red urine or black feces?” “Did you have blood in your vomit or a cough with blood?” “Have you had severe headaches, convulsions (seizures), changes in vision, numbness or tingling in your arms or legs, or a feeling of extreme tiredness, weakness, or nausea?” “Have you had any bleeding from the cut or injury that doesn’t stop or slow down?” |
| Expectations | Explore what the patient is hoping to get out of the consultation | “What were you hoping we’d discuss today?” |
Analysis of earlier, current INR results, apropriate INR target range and current warfarin dosing
- Analysis of earlier, current INR results, apropriate INR target range and current warfarin dosing
- Evaluate previous warfarin dosages
- Evaluate the patient’s earlier INR results
- Assess the patient’s apropriate INR target range
- Evaluate the results of the current INR
Target INR ranges
The most common target INR is 2.5. Others are:
| Recurrent VTE (DVT or PE) despite adequate anticoagulation | 3.5 |
| Cardioversion | Pre – 3.0 Post – 2.5* |
| Mechanical Heart Valves | See below |
*The 2016 European Society of Cardiology (ESC) guidelines on cardioversion state that patients who have been in AF for longer than 48 hours should start OAC therapy at least 3 weeks before cardioversion and continue for 4 weeks afterward (in those without a need for long-term anticoagulation).
Atrial fibrillation Anticoagulation is normally offered to patients with a CHADSVASc score ≥ 2 and considered in men with a CHADSVASc score of 1.
Warfarin is not usually indicated for ischaemic stroke without atrial fibrillation (except in antiphospholipid syndrome), retinal vessel occlusion, peripheral artery thrombosis, coronary artery graft or coronary angioplasty, and stents.
Cardioversion
Anticoagulation for 4 weeks before and for 3 months afterward. To minimize cardioversion cancellations due to low INRs on the day of the procedure we recommend a target INR of 3.0 prior to the procedure and 2.5 afterward (Oxford guidelines).
*The 2016 European Society of Cardiology (ESC) guidelines on cardioversion state that patients who have been in AF for longer than 48 hours should start OAC therapy at least 3 weeks before cardioversion and continue for 4 weeks afterward (in those without a need for long-term anticoagulation).
Mechanical Heart Valves. Target INR range based on indications
| Target INR in mechanical heart valve replacement Mechanical Prosthesis thrombogenicity* | Isolated Aortic Valve Replacement | Mitral or Tricuspid Valve Replacement, or |
| No risk factors** | AVR with Risk factors ** | |
| Low (most current valves) | 2.5 | 3.0 |
| Medium | 3.0 | 3.5 |
| High | 3.5 | 3.5*** |
*Prosthesis thrombogenicity:
- Low: Carbomedics (aortic position), Medtronic Hall, St Jude Medical (without silzone)
- Medium: Bjork-Shiley, other bileaflet valves
- High: Starr-Edwards, Omniscience, Lillehei-Kaster.
**Patient-related risk factors for thrombosis:
- Mitral, tricuspid or pulmonary position
- Previous arterial thromboembolism
- Atrial fibrillation
- Left atrium diameter >50 mm
- Mitral stenosis of any degree
- Left ventricular ejection fraction< 35%.
***Was 4.0 in ESC guideline
Analysis of the factors that may affect the increased INR level
- Assess the presence of warfarin taking errors, low patient compliance, the complexity of the warfarin regimen for the patient
- Assess any changes in the patient’s clinical condition
- Evaluate any changes in medication
- Evaluate any changes in lifestyle
- Evaluate changes in alcohol consumption
It is necessary to clarify with the patient what doses he/she has taken in the last two weeks and to review the dosing schedule.
Ask the patient to bring all their drugs and a box of pills to make sure the drug is correct and the dosage regimen is appropriate.
COMMON CAUSES OF HIGH INRs
| NON‐COMPLIANCE OR ERRORS IN DOSING (The patient mistakenly took a different dosage regimen than was prescribed) | – Complex regimen – Splitting tablets – Dosing error or duplication – Multiple tablet strengths |
| DRUG THERAPY CHANGES, DRUG INTERACTIONS | – Warfarin dose recently altered – Recent antibiotic use – OTC or herbal product added, deleted, or dose altered – Medication added, deleted, or dose altered |
| LIFESTYLE CHANGES, MALNUTRITION (vitamin K deficiency) | – Increase in alcohol use or binge drinking; – Decrease in consumption of Vitamin K containing foods; – Chewing tobacco use recently decreased or discontinued; |
| ALTERED HEALTH STATES | – Fever, acute illness, diarrhea, – Reduced food intake – Uncontrolled hyperthyroidism – CHF exacerbation – Liver disease |
The patient should be asked the following questions to assess the factors that may lead to an INR increase
| NON‐COMPLIANCE OR ERRORS IN DOSING | “Do you have difficulties in taking warfarin?” “Do you understand the warfarin dosing regimen that was prescribed for you?” “Do you understand the warfarin dosing regimen?” “Aren’t you confused about taking warfarin?” “Is it difficult to take your recommended warfarin dosage regimen?” “What dosages of warfarin have you been taking lately?” “Is it convenient for you to divide warfarin tablets in half?” “Do you remember the mistakes in taking warfarin?” “Can you mention the mistakes in warfarin?” “Do you remember days when you took a double dose of warfarin?” “Do you remember days when you mistakenly took more warfarin than you were prescribed?” “Are you experiencing any inconvenience due to the variety of warfarin dosing regimens?” “Do you have difficulties with different warfarin regimens on different days?” “Are you confusing about the dosing regimens that you assigned on certain days?” “Is it convenient for you to divide warfarin tablets in half?” “Do you remember the mistakes in taking warfarin?” “Can you mention the mistakes in warfarin?” “Do you remember days when you took a double dose of warfarin?” “Do you remember days when you mistakenly took more warfarin than you were prescribed?” “Are you experiencing any inconvenience due to the variety of warfarin dosing regimens?” “Do you have difficulties with different warfarin regimens on different days?” “Are you confusing about the dosing regimens that you assigned on certain days?” |
| DRUG THERAPY CHANGES, DRUG INTERACTIONS | “Have you recently had increasing in your warfarin dosage?” “Has there been a recent adjustment of warfarin dosage?” “Have you had a recent concomitant use of antibiotics and other drugs?” “Have you been prescribed antifungals, sulfamethoxazole and trimethoprim, and other drugs?” “Have you had a recent concomitant use of amiodarone?” “Have you had a recent concomitant use of paracetamol or combination drugs containing paracetamol?” “Have you had an acute respiratory illness that required paracetamol or a combination of paracetamol-containing drugs?” “Have you taken drugs to reduce the acidity of gastric juice?” “Have you taken heartburn remedies?” “Have you taken antidepressants?” “Did you take statins or fibrates?” “Have you confessed to acarbose or lactulose?” “Didn’t you use phenytoin?” “Did you have any recent additions, withdrawals, or changes in over-the-counter or herbal dosage regimens?” “Have you had any recent additions, withdrawals, or changes in the dosage regimen of concomitant therapy?” “Didn’t you take thyroid hormones?” Have you been prescribed vitamin E? ” “Have you been prescribed painkillers?” “Have you been prescribed allopurinol?” “Have you been vaccinated?” “Have you used tramadol, oxandrolone?” |
| LIFESTYLE CHANGES, MALNUTRITION (vitamin K deficiency) | “Have you had an increase in alcohol or binge drinking lately?” “Have you had a reduction in your intake of foods containing vitamin K?” “Has there been a decrease in the consumption of products containing vitamin K, such as pickles (fennel), mayonnaise, soybean oil, broccoli, Brussels sprouts, cabbage, leafy greens, kale, lettuce, parsley, spinach, watercress (raw)? » “Have you used cranberries (eg juice, supplements)?” “Did you drink grapefruit or grapefruit juice?” “Has your chewing tobacco consumption decreased or stopped lately?” |
| ALTERED HEALTH STATES | “Have you had a fever lately?” “Have you had an acute illness lately?” “Have you had diarrhea recently?” “Have you had a reduction in food intake?” “Do you suffer from hyperthyroidism? Are you receiving treatment for hyperthyroidism? Do you see an endocrinologist about this? Do you monitor your thyroid function? ” “Has your condition been deteriorating lately?” “Do you have liver disease?” “Has your shortness of breath gotten worse?” “Has your exercise tolerance decreased in recent times?” “Did your lower extremities swell?” “Have you had a feeling of shortness of breath lately?” “Do you need to sit down at night due to lack of air?” |
Hyperthyroidism and fever
Both hyperthyroidism and fever result in a hypermetabolic state, which may accelerate the clearance of vitamin K-dependent clotting factors. Thus the amount of warfarin required to produce an anticoagulant effect would decrease. This means when a patient starts to take carbimazole or propylthiouracil to correct their thyroid function, their warfarin requirement will increase as their thyroid function normalizes.
Liver disease
The use of warfarin in patients with severe liver disease is contraindicated due to the unpredictable effects of liver disease on coagulation, such as:
- vitamin K deficiency due to intra- or extra-hepatic cholestasis
- reduced synthesis of coagulation factors due to severe hepatocellular damage
- functional abnormalities of platelets and fibrinogen found in many patients with
Congestive heart failure
Heart failure can cause hepatic congestion of blood flow and inhibit the metabolism of warfarin leading to excessive anticoagulation with a risk of bleeding. This can be troublesome in patients with frequent exacerbations of heart failure (ie, worsening of heart failure, usually requiring hospitalization).
Providing medical care to the patient if necessary
- Assess the patient’s bleeding and its severity if necessary
- In case of active bleeding, provide immediate medical care after taking INR results
- In the absence of bleeding adjust the dosage of warfarin
Criteria for assessing the severity of bleeding (American College of Cardiology, 2020):
- destabilization of hemodynamics (SBP <90 mm Hg; decrease in SBP ˃40 mm Hg; drop in SBP ≥20 mm Hg or BP ≥10 mm Hg when moving to vertical position; diuresis <0.5 ml/kg/h);
- bleeding in the critical area (intracranial hemorrhage – intracerebral, subdural, epidural, subarachnoid; other hemorrhages of the central nervous system – intraocular, interracial and extra-axial spinal hemorrhage; hemo tamponade; hemothorax, intra-abdominal and extra-abdominal hemorrhage; pulmonary hemorrhage, posterior epistaxis; intramuscular and intra-articular bleeding);
- clinically significant bleeding with a decrease in hemoglobin ≥2 g/dl (20 g/l) or requiring transfusion of ≥2 packets of erythrocyte mass.
If at least one of the above criteria is present, the bleeding is assessed as severe.
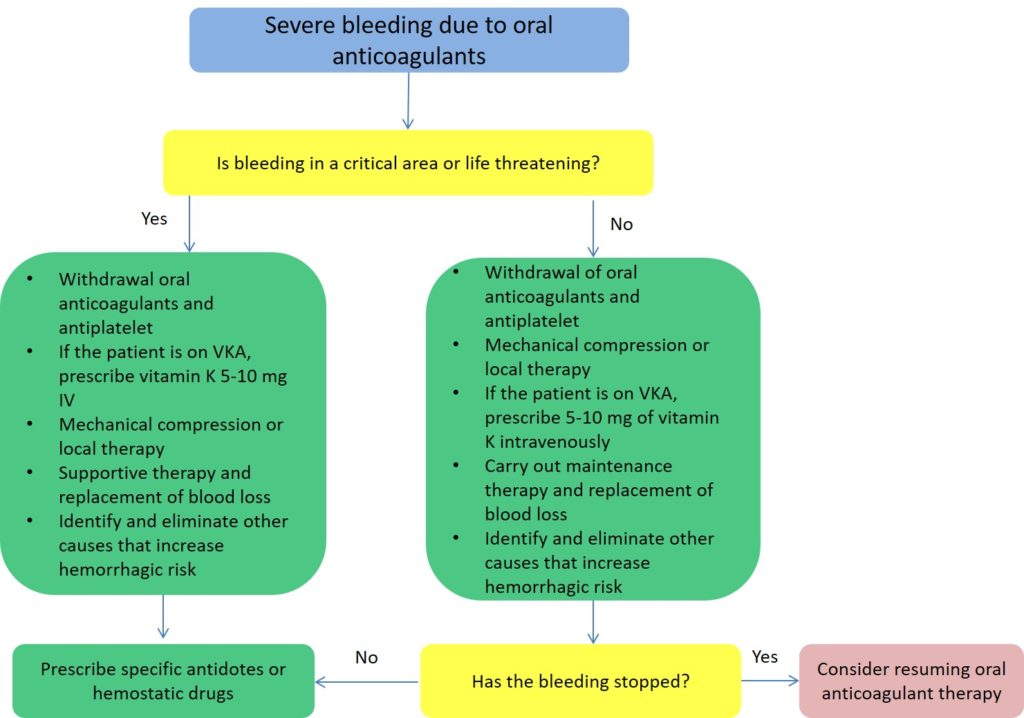
Algorithm for managing a patient with severe bleeding
Algorithm for managing a patient with minor bleeding
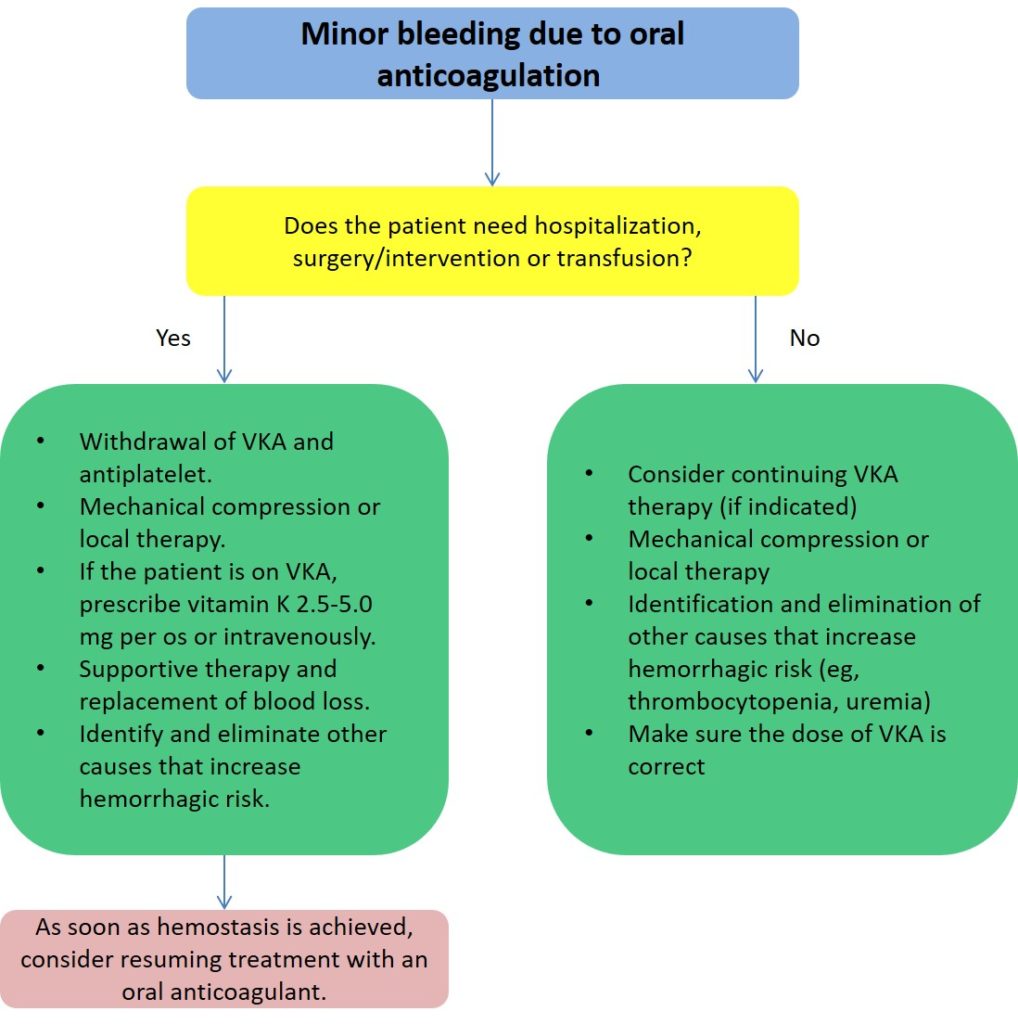
According to the recommendations of the European Society of Cardiology (2020), there is mild, moderate, and life-threatening bleeding. Further tactics of the patient depend on the severity of bleeding and the type of oral anticoagulant.
Algorithm for managing a patient with bleeding with VKA
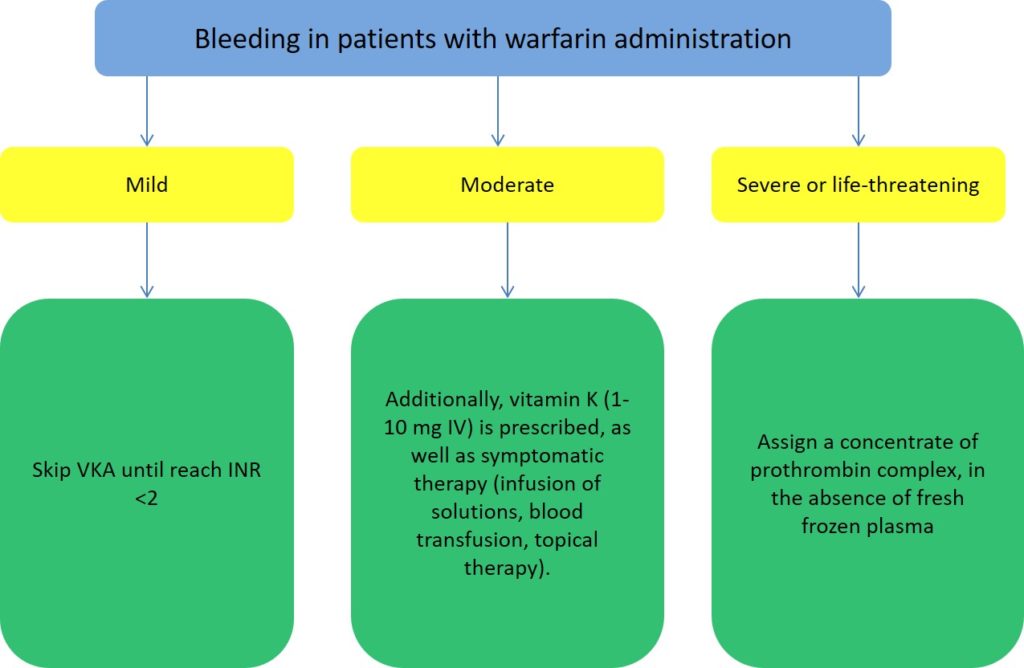
Vitamin K is a specific antidote to vitamin K antagonists (warfarin and other coumarins), the drug has a dose-dependent effect, administered orally, intravenously at a dose of 1 to 10 mg. Slow intravenous infusion shows a more controlled and rapid effect (significant reduction in INR occurs within 4-6 hours) compared to other routes of administration.
In the case of severe bleeding in a patient taking VKA, preference is given to a 4-factor concentrate of prothrombin complex, but not to vitamin K.
Vitamin K1 is an effective antidote to the anticoagulant effect of warfarin. Despite this, data are lacking to show that its use improves outcomes in life-threatening bleeds. While intravenous or oral routes of administration can be used and are effective in reversing an INR that is raised because of warfarin therapy, the intravenous route achieves a more rapid response compared with oral administration, with an onset of action seen within 6–8 hours. However, both routes achieve a similar correction of INR by 24 hours.
Vitamin K1 should not be administered by subcutaneous or intramuscular routes.
Subcutaneous administration is no more effective than placebo, while intramuscular injection in an over-anticoagulated patient may lead to hematoma and bleeding, and its effect on reversal is unpredictable owing to variable absorption – it can be associated with a prolonged increase of vitamin K1 plasma levels, which may hinder re-anticoagulation. The major concern about intravenous vitamin K1 has been anaphylaxis. Although the absolute incidence is unknown, it is most likely rare. There is no convincing association between anaphylaxis and dose, concentration, or rate of administration of vitamin K1 but the literature suggests that current formulations with mixed micelles of lecithin and glycol are safer than the previous preparations containing polyethylene castor oil.
The 4-factor concentrate of the prothrombin complex contains 4 coagulation factors – II, VII, IX, X, as well as protein C and protein S. The required dose of concentrate depends on the level of INR and bodyweight of the patient: at INR 2-4 – 25 IU/kg is recommended; at INR 4-6 – 35 IU/kg is recommended; at INR> 6 – 50 IU/kg is recommended; the maximum possible dose for administration is 5000 IU.
Advantages of 4-factor prothrombin complex concentrate over FFP include rapid reconstitution into a small volume for infusion over 20–30 minutes, fast onset of action, no requirement to check a patient’s blood group, minimal risk of viral transmission due to pathogen reduction and inactivation steps during manufacturing, and reduced risk of other clinical adverse reactions such as transfusion-associated circulatory overload or transfusion-associated acute lung injury. The latter is due to circulating antihuman leukocyte antigen or antigranulocyte antibodies in plasma. However, the 4-factor prothrombin complex concentrate does contain small amounts of heparin, and its use to reverse warfarin anticoagulation should be carefully considered in patients with heparin-induced thrombocytopenia.
FFP contains all coagulation factors present in whole blood but it is not a factor concentrate, and multiple units may be needed if FFP alone is used for warfarin reversal. In addition to the inherent risks of plasma use mentioned already, requirements for its use include the need to determine the patient’s blood group (or to use group AB plasma), appropriate facilities for frozen plasma storage and thawing, and the time taken for infusion. Therefore, FFP should not be used routinely to reverse warfarin anticoagulation; however, where 4-factor prothrombin complex concentrate is unavailable and an emergency reversal is required, FFP should be used, along with vitamin K1 to sustain the reversal effect. Treating a patient with bleeding, regardless of INR For patients on warfarin therapy with bleeding in whom the aim is to normalize the INR, vitamin K1 given intravenously is the preferred treatment because of its faster and predictable onset of action. For this indication, doses 3 mg are ineffective. Consistent with other guidelines, we recommend a dose of 5–10 mg. For life-threatening (critical organ) and clinically significant bleeds, the consensus is to use the maximum dose of 4-factor prothrombin complex concentrate (with vitamin K1 and FFP) and the maximum amount of FFP when 4-factor prothrombin complex concentrate is unavailable.
Among patients with an elevated INR up to 10.0 who do not have bleeding or risk factors for major bleeding, it has been shown that oral administration of low-dose vitamin K1 does not lower the risk of bleeding compared with placebo and should not be used routinely.36 However, for patients with risk factors for bleeding, vitamin K1 1–2 mg orally or 0.5–1.0 mg intravenously should be considered. Risk factors for major bleeding include a major bleed within the previous 4 weeks, surgery within the previous 2 weeks, a platelet count less than 50×109/L, known liver disease, or concurrent antiplatelet therapy. There are no randomized studies to guide the management of patients whose INR exceeds 10.0 and who are not bleeding. A recent single-arm study involving outpatients with an INR greater than 10.0 reported a low rate of major bleeding when these patients received 2.5 mg of oral vitamin K1. Many patients on warfarin are outpatients and information on individual patient bleeding risk is frequently not available to laboratory staff who are involved in reporting elevated INR results and attempting to communicate results to patients. In these settings, good communication between clinical and laboratory staff is essential.
The recommended dose of 4-factor prothrombin complex concentrate to reverse the anticoagulant effect of warfarin according to the initial and target international normalized ratio (INR / INR) *
| Initial INR | ||||
| Target INR | 1.5–2.5 | 2.6–3.5 | 3.6–10.0 | > 10.0 |
| 0.9–1.3 | 30 IU/kg | 35 IU/kg | 50 IU/kg | 50 IU/kg |
| 1.4–2.0 | 15 IU/k | 25 IU/kg | 30 IU/kg | 40 IU/kg |
*Intern Med J 2011; 41: 337-343
Fresh-frozen plasma is prescribed in the absence of a 4-factor concentrate of prothrombin complex.
Fresh frozen plasma contains all the components of the coagulation system and the necessary proteins, but before administration, it is necessary to determine the patient’s blood group according to the ABO system, so the beginning of plasma infusion is often delayed. 10-15 ml/kg of plasma are entered. The following side effects may occur volume overload, allergic reactions, and others.
Characteristics of 4-factor concentrate of prothrombin complex and fresh-frozen plasma
| Four-Factor Prothrombin Complex Concentrate (4F-PCC) | Fresh frozen plasma | |
| Description | Prepared from plasma collected from voluntary donors. Sterile freeze-dried powder containing coagulation factors II, IX, and X and low levels of factor VII | Separated and frozen within 18 hours of collection from volunteer donors. Contains all coagulation factors |
| Contraindications | Patients showing signs of thrombosis or disseminated intravascular coagulation | Do not use when coagulopathy can be corrected more effectively with specific therapy, such as vitamin K1, cryoprecipitate or other specific factor concentrates |
| Specifications | Available in vials containing 500 IU of factor II, IX, and X to be reconstituted in 20 mL of water for injections. Each vial also contains 25 IU of antithrombin and 192 IU of heparin | Available in Australia in units of 250–334 mL and in New Zealand as 180–300 mL (typically 240–275 mL). It May be stored in a monitored blood refrigerator at 2–6°C for up to 5 days once thawed, and relabelled “thawed plasma” in accordance with Australian and New Zealand Society of Blood Transfusion Guidelines. Thawed plasma has levels of factors II, VII, IX, and X adequate for warfarin reversal |
| Availability | From relevant blood service or hospital blood bank | From relevant blood service or hospital blood bank |
| Considerations for use | No need to consider the ABO blood group | Available in all ABO blood groups and should be ABO-group compatible with patient’s red cells (or use AB plasma) |
| Known allergies to prothrombin complex concentrate | The most common adverse events — are allergic reactions and volume overload. Potential for transfusion-related acute lung injury and other transfusion reactions, including the transmission of infections | |
| Predisposition to venous thrombosis disseminated intravascular coagulation, and myocardial infarction | ||
| Heparin-induced thrombocytopenia |
Management of patients on warfarin therapy with bleeding*
| Clinical setting | Recommendations and levels of evidence† |
| INR ≥1.5 with lifethreatening‡ (critical organ) bleeding | Cease warfarin therapy and administer: • vitamin K1 5.0–10.0 mg IV (2C) • and Prothrombinex-VF 50.0 IU/kg§ IV • and fresh frozen plasma 150–300 mL • If Four-Factor Prothrombin Complex Concentrate (4F-PCC) is unavailable, administer fresh frozen plasma 15 mL/kg |
| INR ≥2.0 with clinically significant bleeding (not life-threatening) | Cease warfarin therapy and administer: • vitamin K1 5.0–10.0 mg IV (2C) • and Prothrombinex-VF 35.0–50.0 IU/kg IV according to INR • If Four-Factor Prothrombin Complex Concentrate (4F-PCC) is unavailable, administer fresh frozen plasma 15 mL/kg |
| Any INR with minor bleeding | Omit warfarin, repeat INR the following day and adjust warfarin dose to maintain INR in the target therapeutic range (2C) • If the bleeding risk is high** or INR > 4.5, consider vitamin K1, 1.0–2.0 mg orally or 0.5–1.0 mg IV |
INR = international normalised ratio. IV = intravenously. * Indication for warfarin therapy should be reviewed; if clinically appropriate, consider permanent cessation. † Level of evidence in parentheses in bold. ‡ Includes intracranial bleeding. § Consider administering a Four-Factor Prothrombin Complex Concentrate (4F-PCC) dose less than 50.0 IU/kg when INR 1.5–1.9. ** Recent major bleed (within previous 4 weeks) or major surgery (within previous 2 weeks), thrombocytopenia (platelet count, < 50×109/L), known liver disease, or concurrent antiplatelet therapy
Management of patients on warfarin therapy with high INR and no bleeding
| Clinical setting | Recommendations and levels of evidence* |
| INR<4.5 and no bleeding | Lower or omit the next dose of warfarin Resume therapy at a lower warfarin dose when the INR approaches the therapeutic range |
| INR 4.5–10.0 and no bleeding | • If the INR is only minimally above therapeutic range (up to 10%) dose reduction is generally not necessary (2C) • Cease warfarin therapy; consider reasons for elevated INR and patient-specific factors. Vitamin K1 is usually unnecessary (2C) • If the bleeding risk is high:† consider vitamin K1 1.0–2.0 mg orally or 0.5–1.0 mg IV • measure INR within 24 h • resume warfarin at a reduced dose once INR approaches therapeutic range |
| INR > 10.0 and no bleeding | • Cease warfarin therapy, administer 3.0–5.0 mg vitamin K1 orally or IV‡ (2C) • Measure INR in 12–24 h. Close monitoring of INR daily to second daily over the following week • Resume warfarin therapy at a reduced dose once INR approaches therapeutic range • If the bleeding risk is high:† consider Four-Factor Prothrombin Complex Concentrate (4F-PCC), 15–30 IU/kg • measure INR in 12–24 h. Close monitoring over the following week • resume warfarin therapy at a reduced dose once INR approaches the therapeutic range |
INR = international normalised ratio. IV = intravenously. * Level of evidence in parentheses in bold; details. Recommendations with no evidence level are standard practice and not based on gradable evidence. † Recent major bleed (within previous 4 weeks) or major surgery (within previous 2 weeks), thrombocytopenia (platelet count, < 50х109/L), known liver disease, or concurrent antiplatelet therapy. ‡ Extrapolated from oral vitamin K data in absence of IV data.
Bleeding whilst taking warfarin
- Explain that the main side effect of warfarin is bleeding more easily than normal
- Explain the common types of ‘less serious bleeding’ and what to do if they experience them
- Explain the rarer types of ‘serious bleeding’ and what to do if they experience them
The main side effect of warfarin involves bleeding more easily than normal (e.g. epistaxis, bleeding gums, heavier periods, bruising). These side effects most commonly occur in the first few weeks of treatment or when the patient is unwell. It is important to discuss the different types of bleeding the patient may experience and inform them what to do in these situations.
| Less serious bleeding Minor bleeding | Serious bleeding Major bleeding |
| “It is normal to bleed more easily when taking warfarin as the medication works by thinning the blood. Common types of bleeding include – periods that are heavier and last longer than normal – bleeding for a little longer than usual if you cut yourself – occasional nosebleeds (that last for less than 10 minutes) – bleeding from your gums when you brush your teeth – bruised that come up more easily and take longer to fade than usual. This type of bleeding is not dangerous and should stop by itself. If it happens, keep taking the warfarin, but tell your doctor if the bleeding bothers you or does not stop.” | “Occasionally, you can have serious bleeding from taking warfarin. This can be dangerous and needs urgent medical attention.” “Stop taking warfarin and call your doctor or anticoagulant clinic, or go to A&E if you experience: – red pee or black poo, – large bruises or bruises that happen for no reason, – nosebleeds that last longer than 10 minutes, – blood in your vomit or you’re coughing up blood, – severe headaches, fits (seizures), changes to your eyesight, numbness or tingling in your arms or legs, or feeling very tired, weak, or sick – these can be signs of bleeding in your brain – any bleeding from a cut or injury that will not stop or slow down” |
How to take warfarin
- Explain that warfarin should be taken at the same time each day
- Explain the different types of warfarin tablets
- Explain what the patient should do if they forget a dose
- Advise the patient to let medical professionals know that they take warfarin when they are being prescribed new medications
- Advise the patient to let the team managing their anticoagulation know when they start taking a new medication
- Advise the patient about the importance of effective contraception if taking warfarin (if relevant)
Key points to communicate when discussing warfarin use:
- “Warfarin should be taken at the same time each day to keep the levels of warfarin steady.”
- “Tablets have different colours depending on their strength (e.g. 0.5mg white; 1mg brown; 3mg blue; 5mg pink).”
- “If you forget to take a dose you should take it as soon as you remember, but if you don’t remember till the following day you should skip the missed dose. You should never take two doses together to make up for a missed dose and you should inform your doctor or warfarin clinic about any missed doses at your next appointment.”
- “Whenever you are going to purchase or be prescribed a new medication you should let the doctor or pharmacist know that you take warfarin so they can avoid prescribing medications which alter your warfarin level.”
- “When you start taking a new medication you should let your doctor or anticoagulant clinic know so that they can consider if your warfarin levels need monitoring more frequently.”
- “You should continue to take your warfarin tablets regularly until you have been told to stop.”
- “Warfarin is not safe to be used during pregnancy and therefore you should have an effective contraceptive method in place before you start taking warfarin.”
- “You must inform anticoagulant healthcare staff if you think you have taken too much warfarin or have missed any doses.”
- “You must inform the relevant healthcare professionals if you start, stop or change the dose of your medicines, or if your diet changes substantially (eg. intake of broccoli, lettuce or spinach /)”Other medicines” include not only prescribed drugs but also products that may be brought without prescription, such as aspirin, and medicines containing aspirin, vitamins, food supplements and herbal or homoeopathic remedies.”
- “If you require surgery, dental work, or any other invasive procedure you may need stop taking warfarin temporarily. You should discuss your warfarin management with a healthcare professional prior to the procedure”.
Tips for further warfarin dosing according to the analysis of the reasons that led to the INR levels increase
- Estimate the required duration of administration of a concomitant drug that interacts with warfarin (temporary, chronic) as needed
- Adjust warfarin dosage as needed
- Withdraw warfarin if necessary
- Evaluate the rationality and necessity of co-administration of antiplatelet agents and nonsteroidal anti-inflammatory drugs if necessary
- Most common drugs that can increase INR:
- Antibiotics: sulfamethoxazole/trimethoprim, metronidazole, quinolones (ciprofloxacin, levofloxacin), amoxicillin, erythromycin, clarithromycin, azithromycin
- Azole antifungals: fluconazole, miconazole, voriconazole
- Cardiac drugs: amiodarone, some statins (fluvastatin), fenofibrate
- Acetaminophen >1 g/day
- Levothyroxine dose increases – full effect observed after 4‐6 weeks of dose change
- Management strategy:
- If the interacting drug is temporary and significantly increases the INR, may temporarily hold and/or reduce the maintenance dose of warfarin until the interacting effect resolves.
- If the interacting drug will be used chronically, modify the warfarin dose according to a
- dosing nomogram.
- Although warfarin interacts with many drugs, virtually no drug requires complete avoidance in a patient who is also taking warfarin therapy (or vice versa). Increasing the frequency of INR tests, initially, allows for appropriate dosing adjustments, if necessary.
- There may be some exceptions to this approach. For example, patients receiving chemotherapy with emesis or infection may have INR fluctuation that is difficult to control.
- In such cases, switching the patient to a low molecular weight heparin (LMWH) until stabilization of the underlying condition is suggested.
- Note: Antiplatelet agents (acetylsalicylic acid [ASA], clopidogrel, prasugrel, ticagrelor) and Non‐steroidal Anti‐Inflammatory Drugs (NSAIDs) significantly increase the risk of bleeding when combined with warfarin but generally do not change the INR. The indication and clinical necessity of using these agents should be carefully weighed against the increased bleeding risk.
Strategy approach in a patient with altered health states
- Transient infectious illness (fever and/or diarrhea):
- Fever increases the metabolic state which may result in depletion of clotting factors and increased INR.
- Being ill can also alter diet and may lead to a transient vitamin K deficiency.
- Uncontrolled hyperthyroidism – leads to increased clearance of clotting factors, resulting in high INR.
- Congestive heart failure (CHF) exacerbation (perhaps due to liver congestion).
- Management Strategy:
- Temporarily reduce the warfarin dose and increase the frequency of INR monitoring until the patient’s health state stabilizes
Algorithm for warfarin dose adjusting
It may be necessary to (temporarily) reduce the dose of warfarin and/or skip one or two doses based on the assessment of INR level. The INR should be re-measured to be sure about its decreasing after two or three days.
| INR | Recommended dose adjustment of warfarin |
| <1.5 | Increase the weekly dose by 10-20% Consider additional doses INR control in 4-8 days under the doctor consideration |
| 1.5 to <2 | Increase the weekly dose by 10-20% INR control in 4-8 days under the doctor consideration |
| 2.0-3.0 | Unchanged |
| >3.0 to 3.5 | Decrease the weekly dose by 10-20% INR control under the doctor consideration |
| 4.0 to >5.0 | Skip 0 to 1 dose and/or reduce the weekly dose by 0-20% INR control under the doctor consideration |
| >4.0 but >5.0 | Skip 1-2 doses and reduce the weekly dose by 10-20% INR control in 3-7 days under the doctor consideration |
| 5.0 to >9.0 without significant bleeding | Skip 1-2 doses INR control in 1-2 days under the doctor consideration To resume warfarin taking when INR <3.0 with a decrease in a weekly dose by 5-20% If urgent surgery is required, the patient should be given fresh-frozen plasma |
| ≥9.0 without significant bleeding | Do not take warfarin Assign vitamin K (2.5-5 mg orally once) INR control daily to > 3.0, reducing the weekly dose by 10-20% If urgent surgery is required, the patient should be given fresh-frozen plasma |
Altered Nutritional Status
- Patients who are malnourished are commonly vitamin K deficient.
- Sudden changes in diet may be due to social circumstances such as a death of a spouse/family member/pet or stressful work or health situations.
- Management Strategy:
- Ask the patient to describe their eating pattern and intake.
- Recommend eating consistent meals or use of a meal replacement beverage (e.g. 4 cans of
- Ensure contain the required daily amounts of nutrients) or multivitamins containing vitamin K.
- If this is not successful, consider lowering the maintenance dose and increasing the frequency of monitoring.
Alcohol consumption
Even a single moderate consumption or a large amount of alcohol consumed (more than two glasses) can temporarily increase the INR level (for example, alcohol consumption on weekends). In case of cessation of alcohol intake, it is possible to continue the usual maintenance dose.
It is recommended alcohol abuse prevention.
Errors in dosing
The patient may have mistakenly taken a different dosage regimen than what was prescribed.
Management Strategy:
- Ask the patient exactly what doses they have taken in the past 2 weeks and review their dosing calendar.
- Ask the patient to bring in all of their medications and pill box to ensure the correct drugs and doses are being taken. If the patient has a good relationship with their local pharmacy, ask the pharmacist to double check.
- Use a warfarin dosing calendar. Encourage the patient to use a calendar to record their INRs and warfarin doses taken.
- Use a warfarin dosette (pill box). The patient or caregiver puts the daily doses in a weekly pill box.
- Simplify the dosing regimen. Use of a single tablet strength to avoid multiple strength confusion and strategically putting extra/reduced daily doses on days that are easy to remember (e.g. “Take 1 tablet every day except take 2 tables on Sundays.”
Lifestyle advice
- Advise the patient about the impact of diet on the effect of warfarin
- Advise the patient about the impact of alcohol on the effect of warfarin
- Advise the patient about brushing teeth, shaving and dental procedures
| Diet | Drastic changes in diet, especially an increase in consumption of foods high in vitamin K (such as broccoli, kale, or spinach) can potentially affect the control of anticoagulation. If the patient ever wishes to significantly change their diet, they should inform the anticoagulant clinic so necessary dose adjustments and monitoring requirements can be fulfilled. “Since vitamin K and warfarin work against each other, the amount of vitamin K in your diet can change warfarin’s effects. It is important to keep your dietary intake of vitamin K consistent. Foods such as green leafy vegetables and certain oils have higher contents of vitamin K. (See the table below for a chart of vitamin K content in selected foods). If you DECREASE your intake of vitamin K (eat fewer foods containing vitamin K) your dose of warfarin may need to be lowered to prevent bleeding. If you INCREASE your intake of vitamin K, your dose of warfarin may need to be increased to prevent blood clots. A MAJOR change in your vitamin K intake can affect your PT/INR, but normal daily variation in the foods you eat is okay. You DON’T have to avoid foods that are high in vitamin K, just keep your diet consistent. You should let your healthcare professional know if there is going to be a major change in your diet, so your PT/INR can be closely monitored” Many people are on special diets, such as the Atkin’s or South Beach diets, to lose weight. These diets are high-protein diets and can also affect the way warfarin works in your body. Once you take a dose of warfarin, some of it binds to protein in your bloodstream. While warfarin is attached to this protein, it has no effect on your body. It’s thought that high protein diets can increase the number of proteins in your body and cause more warfarin to be bound to protein. This causes a DECREASE in warfarin available to prevent clots, so your warfarin dose may need to be increased. Always check with your healthcare professional before starting any special diets, so your PT/INR can be closely monitored. Certain foods can also affect how your liver clears warfarin from your body, causing warfarin levels to increase or decrease. Examples include alcohol, cranberry products (e.g., juice, supplements), and possibly grapefruit or grapefruit juice. Too much alcohol, cranberry products, or grapefruit products can INCREASE warfarin’s effect and increase your risk of bleeding. Avoid or limit your intake of alcohol, cranberry products, and grapefruit or grapefruit juice. Make sure your healthcare professional knows if your diet contains any of these products, so your PT/INR can be closely monitored. Cranberry juice is also known to interact with warfarin and enhance its anticoagulant effect and therefore it should be avoided. “People on vitamin K-rich diets should not change eating habits without at the same time reducing the warfarin dosage, because excessive anticoagulation and bleeding may occur.” |
| Alcohol | Patients should limit their alcohol intake to a maximum of one or two drinks a day and never binge drink. If there are major changes in alcohol consumption (e.g. the patient stops drinking, or starts drinking more) the INR can be affected. “People should limit the amount of alcohol to a maximum of one or two drinks a day and never bridge drink.” |
| Other | Patients should be advised to take extra care when carrying out routine tasks such as brushing teeth or shaving; a soft toothbrush or an electric razor can help. Patients should also be advised to inform their dentist that they take warfarin when booking an appointment as this may have implications for dental procedures. “Other things to remember when taking warfarin In addition to foods, many prescription and over-the-counter drugs, including vitamins and herbal supplements, can affect your warfarin level. You should not start, stop, or change doses of any drugs or supplements without first talking with your healthcare professional. Try to keep a healthy, well-balanced diet and keep your vitamin K intake consistent. Take your warfarin dose around the same time each day. If you miss a dose, take it as soon as you remember. If it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Don’t double up doses without checking with your healthcare professional. Tell your healthcare professional immediately if you have unusual bleeding or bruising, black or bloody stools, blood in the urine, or stomach pain.” “People should avoid activities which could cause abrasion, bruising or cuts (eg., contact sports, gardening, sewing), or at least use protection.” People should avoid insect bites, especially on their legs, and should use a repellent when exposed to insects. Patients with deep vein thrombosis should be given the following additional lifestyle advice: regular walking exercise helps to reduce the risk of further deep vein thrombosis and improves circulation in the affected limb the affected leg should be elevated when sitting “If you are traveling for any length of time will need to move your dosing time gradually – say by an hour a day – to a time that is convenient to the new zone. You may also need to have an INR check while you are away.” |
Yellow booklets and alert card
- Remind the patient with information about the INR monitoring booklet and patient information booklet
- Remind the patient the importance of carrying the anticoagulant alert card with them at all
At the start of treatment, all patients should be provided with two yellow anticoagulant booklets, an INR monitoring booklet, and a patient information booklet. Patients should also be provided with an anticoagulant alert card.
Patients should be advised to always carry the anticoagulant alert card with them in case of an emergency and always take the yellow INR monitoring book with them to each appointment at the anticoagulant clinic and if possible to other appointments (e.g. GP, pharmacy reviews, dental appointments, etc).
The patient information book is a useful resource since it provides the patient with a point of reference and reinforces what has been covered in this guide.
Closing the consultation
- Summarise the key points back to the patient
- Ask the patient if they have any questions or concerns that have not been addressed
- Arrange appropriate follow-up
- Thank the patient for their time
- Dispose of PPE appropriately and wash your hands
Key communication skills
Summarise the key points back to the patient.
Ask the patient if they have any questions or concerns that have not been addressed.
If you feel that the patient would benefit from a recap session, arrange a follow-up appointment (face-to-face or telephone) and also direct the patient to the yellow anticoagulant information booklet for further reading.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Key communication skills
- Active listening
- Summarising
- Signposting
Key clinical skills
- Determining the target INR level depending on the clinical situation
- Analysis of the factors that may affect the INR increase
- Providing medical care to the patient with INR increase
- Advice to the patient and explanations about lifestyle, diet
If necessary, re-detail Counseling a patient who is taking warfarin / OSCE guide
Supplements materials
Principles for preventing high international normalised ratio (INR)
- When starting warfarin therapy, avoid high loading doses of warfarin. In general, it is preferable to start treatment using an initial daily dose of 5 mg, or even lower in elderly patients. However, some guidelines have suggested that patients who are considered sufficiently healthy may receive warfarin 10 mg daily for the first 2 days with subsequent doses to be determined by the INR (2C)
- Consider potential warfarin–drug interactions. Avoid concomitant non-steroidal antiinflammatory drugs and certain antibiotics (2C). Avoid concomitant antiplatelet therapy except where clinical benefit is known, such as mechanical heart valves, acute coronary syndrome, or recent insertion of coronary stents (2C)
- Test the INR more frequently after starting, stopping or changing the dose of concomitant medication
- Avoid frequent dose adjustments. A change in warfarin dose will take several days to influence the INR, so testing the INR within 24 or 48 hours of a dose change may not truly reflect the steady-state response to the dose adjustment
- Avoid excessive increases in dose when the INR drifts below the target INR range
- Effective patient education can minimise compliance problems
- Pharmacogenetic testing to guide warfarin dosing is not necessary (1B)
Vitamin K Content of Selected Foods
* Note: This is NOT a list of foods to avoid. This list provides information on the vitamin K content of certain foods.
| Foods | Low | Moderate | High |
| Vegetables | Green beans | Asparagus | Broccoli |
| Carrots | Avocado | Brussels sprouts | |
| Cauliflower | Red Cabbage | Cabbage | |
| Celery | Green peas | Collard greens | |
| Corn | Endive (raw) | ||
| Cucumber (peel removed) | Pickle (dill) | Kale (raw leaf) | |
| Eggplant | Lettuce (iceberg) | Lettuce (bib, red leaf) | |
| Mushrooms | Mustard greens (raw) | ||
| Onions | Parsley | ||
| Green pepper | Spinach | ||
| Potato | Turnip greens (raw) | ||
| Pumpkin | Watercress (raw) | ||
| Sauerkraut (canned) | Swiss chard | ||
| Tomato | |||
| Fruits | Apple | ||
| Banana | |||
| Blueberries | |||
| Grapes | |||
| Orange | |||
| Meats | Beef | ||
| Chicken | |||
| Pork | |||
| Tuna | |||
| Turkey | |||
| Fats and Oils | Corn oil | Margarine | Mayonnaise |
| Peanut oil | Olive oil | Canola oil | |
| Safflower oil | Soybean oil | ||
| Sesame oil | |||
| Sunflower oil | |||
| Dairy Products | Butter | ||
| Cheese (cheddar) | |||
| Eggs | |||
| Sour cream | |||
| Yogurt | |||
| Beverages | Coffee | ||
| Cola | |||
| Fruit juices | |||
| Milk | |||
| Tea (black) | Tea (green)** |
** There is some controversy as to whether brewing green tea alters the vitamin K content and/or whether green tea may alter the effect of warfarin by some other mechanism
Potential Interactions of Dietary Supplements with Warfarina
| Potential Increase in Risk of Bleeding | ||
| Acetyl-L-carnitine | Fish oil | Mate |
| Arnica | Flaxseed, Flaxseed oil | Melatonin |
| Alcohol, acute use | Fo-ti | Mesoglycan |
| Bishop’s weed | Forskolin | Milk thistle |
| Black tea | Forsythia | N-acetyl glucosamine |
| Bladderwrack | Gamma-linolenic acid | Nattokinase |
| Boldo | Garlic | Oolong tea |
| Borage seed oil | Ginger | Pantethine |
| Burdock | Ginkgo | Papaya |
| Caffeine | Ginseng, Siberian | Peppermint oil |
| Chondroitin sulfate | Glucosamine | Propionyl-L-carnitine |
| Cod liver oil | Grapefruit, Grapefruit juice | Red clover |
| Coltsfoot | Guarana | Reishi mushroom |
| Cranberry, cranberry juice | Guggul | Resveratrol |
| Danshen | Holy basil | Saw palmetto |
| Devil’s claw | Honeysuckle | Sea buckthorn |
| Dong quai | Horse chestnut | Tiratricol |
| Epimedium | Ipriflavone | Turmeric |
| Eucalyptus oil | Jiaogulan | Vinpocetine |
| Evening primrose oil | Kava | Vitamin A |
| Fenugreek | L-carnitine | Vitamin E |
| Feverfew | Lycium | Willow bark |
| Wintergreen | ||
| Possible Decrease in Warfarin’s Effects | ||
| Acerola | ||
| Alcohol, chronic use | ||
| Alfalfa | ||
| Cherokee rosehip | ||
| Chlorella | ||
| Coenzyme Q10 | ||
| Corn silk | ||
| EDTA | ||
| Ginseng, American | ||
| Ginseng, Panax | ||
| Green tea | ||
| Limonene | ||
| Rose hip | ||
| Smartweed | ||
| Soy | ||
| Spinach | ||
| St. John’s wort | ||
| Stinging nettle | ||
| Vitamin C | ||
| Vitamin K | ||
| Watercress |
Related simulation training:
Related articles:
Literature:
- 12020 ACC Expert Consensus Decision Pathway on Management of Bleeding in patients on oral anticoagulants: a report of the American College of cardiology solution set oversight committee. Jam Coll Cardiol. 2020. Aug, Vol.76 (5). 594-622.
- 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACT). Supplementary data. European Heart Journal (2020), 42, 373-498.
- Huyen A Tran et al. Guidelines. An update of consensus guidelines for warfarin reversal. MJA. 2013; Vol.198(4): 7 P. doi: 10.5694/mja12.10614
- What You Should Know About Your Diet and Warfarin. PHARMACIST’S LETTER / Prescriber’s Letter to give to their patients. P.O. Box 8190, Stockton, CA 95208. May 2005 ~ Volume 21 ~ Number 210507, 8 p.
- Beatty SJ, Mehta BH, Rodis JL. Decreased warfarin effect after initiation of high-protein, lowcarbohydrate diets. Ann Pharmacother 2005;39:744
- Committee on Safety of Medicines (CSM). Current Problems in Pharmacovigilance 2003;29:8.
- Shields KM. Possible Cranberry and Warfarin Interaction. Pharmacist’s Letter/Prescriber’s Letter 2003;19(11):191103.
- Havrda DE, Mai T, Chonlahan J. Enhanced antithrombotic effect of warfarin associated with low-dose alcohol consumption. Pharmacotherapy 2005;25:303-7.
- OXFORD HAEMOPHILIA AND THROMBOSIS CENTRE PROTOCOLS FOR OUTPATIENT ORAL ANTICOAGULATION WITH VITAMIN K ANTAGONISTS. Prepared by D. Keeling with input and review from S. Shapiro, N. Curry, V. Price, and L. Mulholland.AC Protocols version 4.1 May 2017
- Paulus Kirchhof, Stefano Benussi, Dipak Kotecha, Anders Ahlsson, Dan Atar, Barbara Casadei, Manuel Castella, Hans-Christoph Diener, Hein Heidbuchel, Jeroen Hendriks, Gerhard Hindricks, Antonis S. Manolis, Jonas Oldgren, Bogdan Alexandru Popescu, Ulrich Schotten, Bart Van Putte, Panagiotis Vardas, Stefan Agewall, John Camm, Gonzalo Baron Esquivias, Werner Budts, Scipione Carerj, Filip Casselman, Antonio Coca, Raffaele De Caterina, Spiridon Deftereos, Dobromir Dobrev, José M. Ferro, Gerasimos Filippatos, Donna Fitzsimons, Bulent Gorenek, Maxine Guenoun, Stefan H. Hohnloser, Philippe Kolh, Gregory Y. H. Lip, Athanasios Manolis, John McMurray, Piotr Ponikowski, Raphael Rosenhek, Frank Ruschitzka, Irina Savelieva, Sanjay Sharma, Piotr Suwalski, Juan Luis Tamargo, Clare J. Taylor, Isabelle C. Van Gelder, Adriaan A. Voors, Stephan Windecker, Jose Luis Zamorano, Katja Zeppenfeld, 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS, EP Europace, Volume 18, Issue 11, November 2016, Pages 1609–1678, https://doi.org/10.1093/europace/euw295
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Checklist – Counseling “Explain a bone marrow aspiration”
IntroductionPointsIntroduces and identifies patient1Gains consent1Explore Checks patients understanding for reason for Bone Marrow Aspiration2Check’s patients understanding…
Checklist – Counseling “History of Acute Intermittent Porphyria”
IntroductionPointsIntroduce and check the details1Consent1Presenting Compliant Elicit intermittent nature of abdominal pain1Details on length of suffering…
Calgary-Сambridge guide to the medical interview
This manual was developed by specialists from the Faculty of Medicine of the University of…
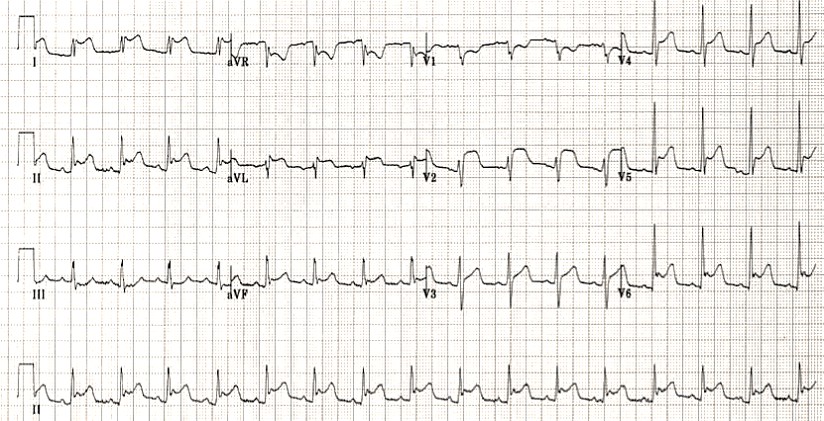
Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents /OSCE guide
Opening the consultationWash your hands and don PPE if appropriateIntroduce yourself to the patient including…
Interactive OSCE Checklist – Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents
Clinical case simulator – Call to Emergency Service from a patient with chest pain (OSCE station)
A team of paramedics urgently arrives on the call to a man who is experiencing…