Aslanger’s Pattern
Introduction
The fourth universal definition of myocardial infarction (MI) defines ST-segment elevation MI (STEMI) and non-STEMI based on the presence or absence of:
1) J-point elevation in two or more contiguous leads with a cut-off value of ≥0.1 mV (1 mm) in all leads other than V2 and V3;
2) STE in V2 and V3 by age and sex, for which the following cut-off values were applied: 0.2 mV (2 mm) in men ≥40 years old, 0.25 mV (2.5 mm) in men <40 years old, or 0.15 mV (1.5 mm) in women.
However, recently, were described new ECG patterns. This definition should be expanded based on the necessity of the wider implementation of the early reperfusion therapy strategies in this group of patients due to the higher mortality in these patients.
Clinical significance
In April 2020, a group of Turkish scientists Aslanger et al. described an ECG pattern, which was recorded according to their data in approximately 13.3% of cases of lower myocardial infarction. Patients with this pattern on the ECG are often incorrectly regarded in the provision of medical care – as patients with ACS without ST-segment elevation, which deprives them of emergency revascularization, while this ECG pattern is associated with coronary artery occlusion in patients with multivessel coronary disease.
Aslanger et al. analyzed the results of ECG and angiography of 1000 patients with STEMI (without ST-segment elevation), 1000 controls (without myocardial infarction), as well as patients with inferior STEMI (with ST-segment elevation) admitted during the same period (DIFOCCULT Study Protocol – DIagnostic accuracy oF electrocardiogram for acute coronary OCClUsion resuLTing in myocardial infarction).
Aslanger’s pattern was observed in 6.3% of patients with STEMI and was a predictor of greater heart attack size and higher mortality.
Aslanger pattern
- Occurs with a combination of lower AMI and critical ischemia of another localization.
- Larger infarction zone, as evidenced by troponin levels at 24 hours, higher incidence of angiographic injury, and higher incidence of the combined endpoint of acute coronary occlusion compared with patients with AMI without ST-elevation.
- High mortality, comparable to patients with inferior STEMI, both in-hospital (5% versus 4%, P = 0.675) and one-year mortality (11% versus 8%, respectively; P = 0.311).
Concomitant multivessel coronary artery disease predisposes these patients to poor outcomes if the time to reperfusion is delayed.
Identifying the culprit during angiography can be difficult if there are multiple critical stenoses, and this specimen will help to expose the lesions that supply the lower wall first.
This pattern occurs with a simultaneous combination of inferior MI and diffuse ischemia due to lesions of the anterior interventricular branch of the left coronary artery (left anterior descending artery), the left main coronary artery, or a three-vessel lesion.
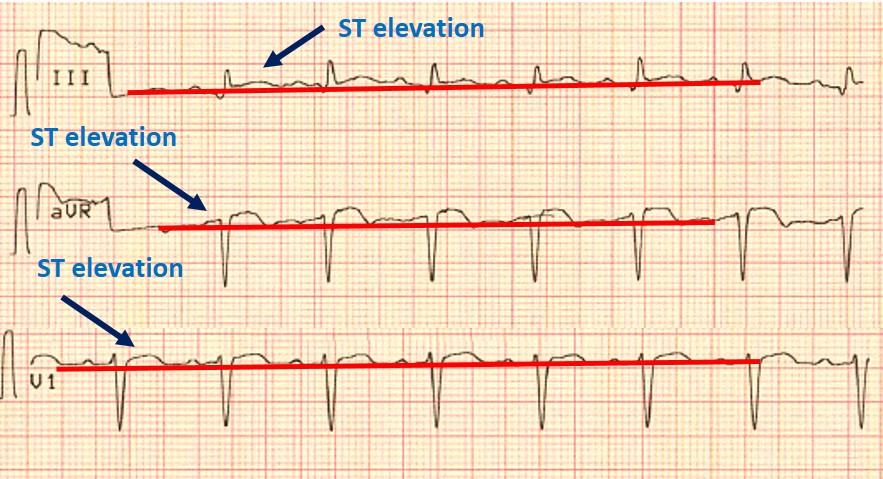
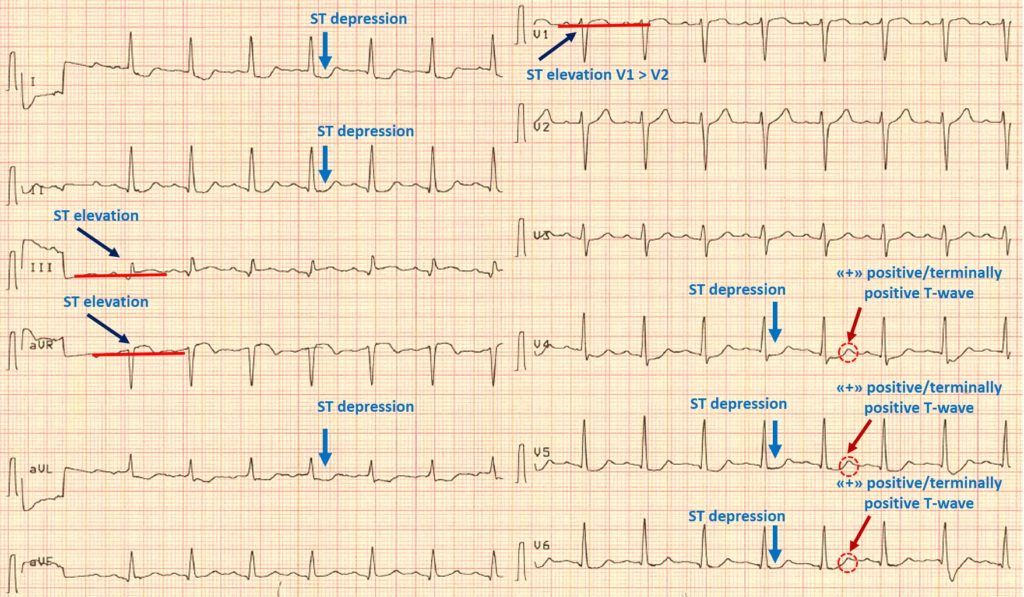
ECG criteria:
1) ST elevation in lead III, but in none of the inferior leads, as well as in aVR and V1.
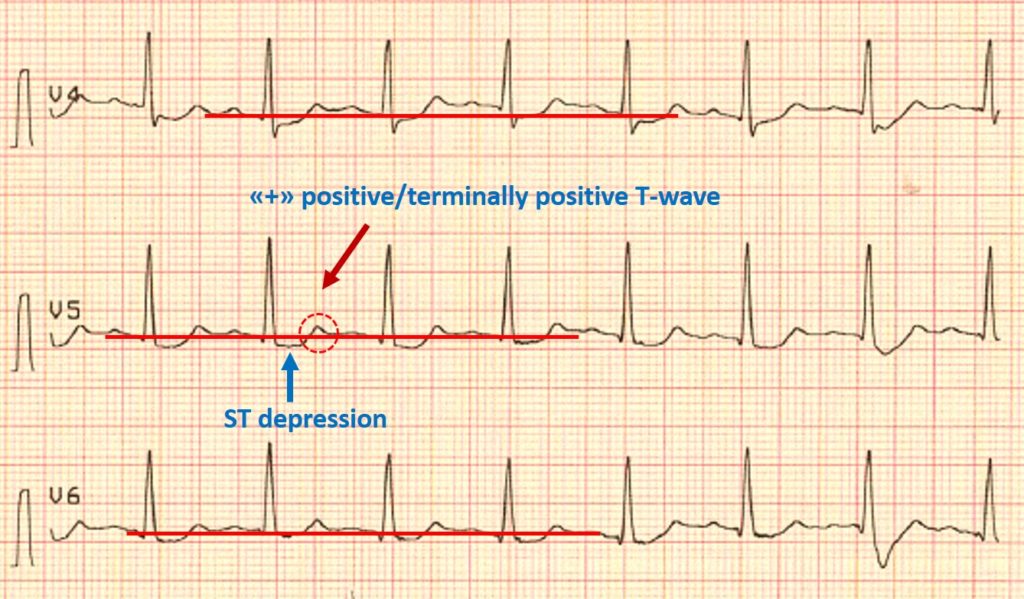
2) Concomitant ST depression in any of V4-V6 with positive / terminally positive T-wave.
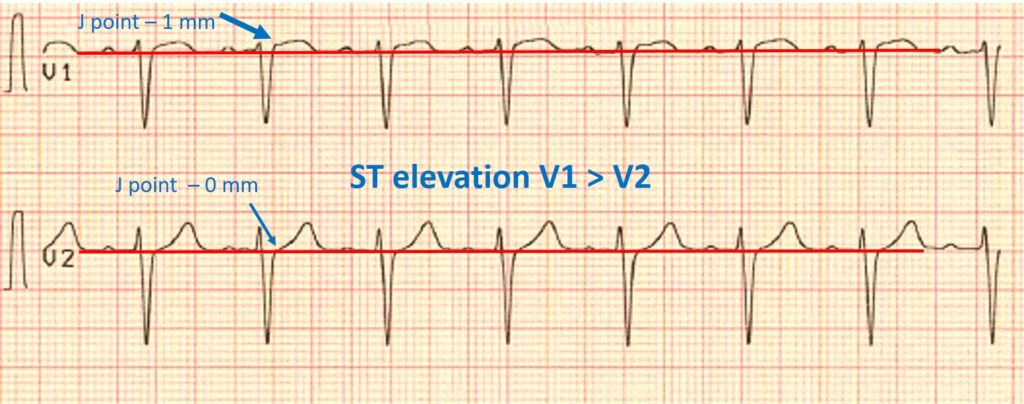
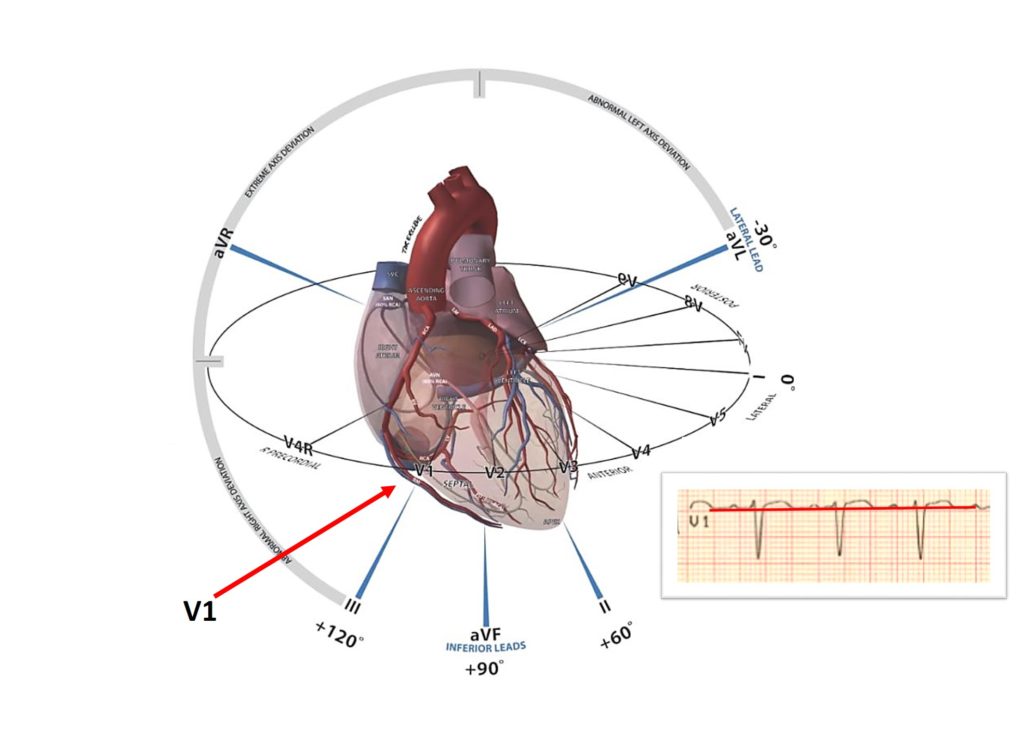
3) ST-segment elevation in V1> V2
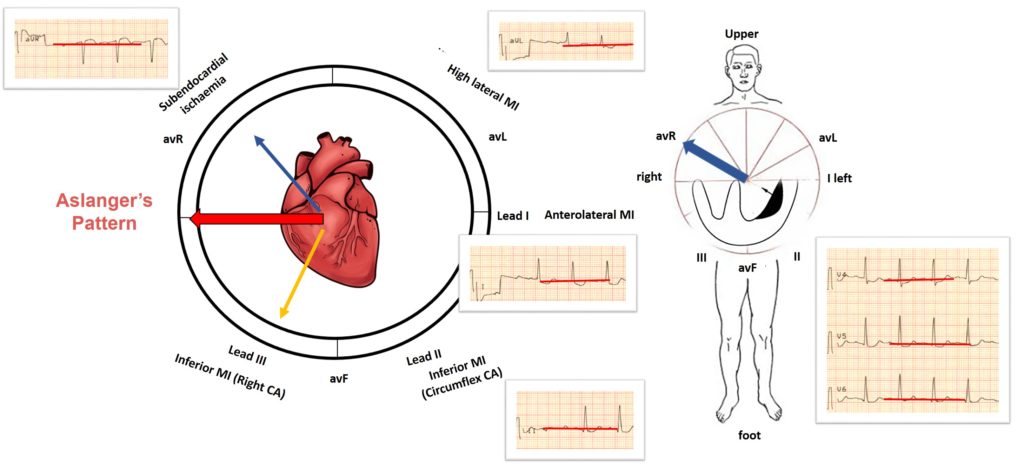
Aslanger’s Pattern
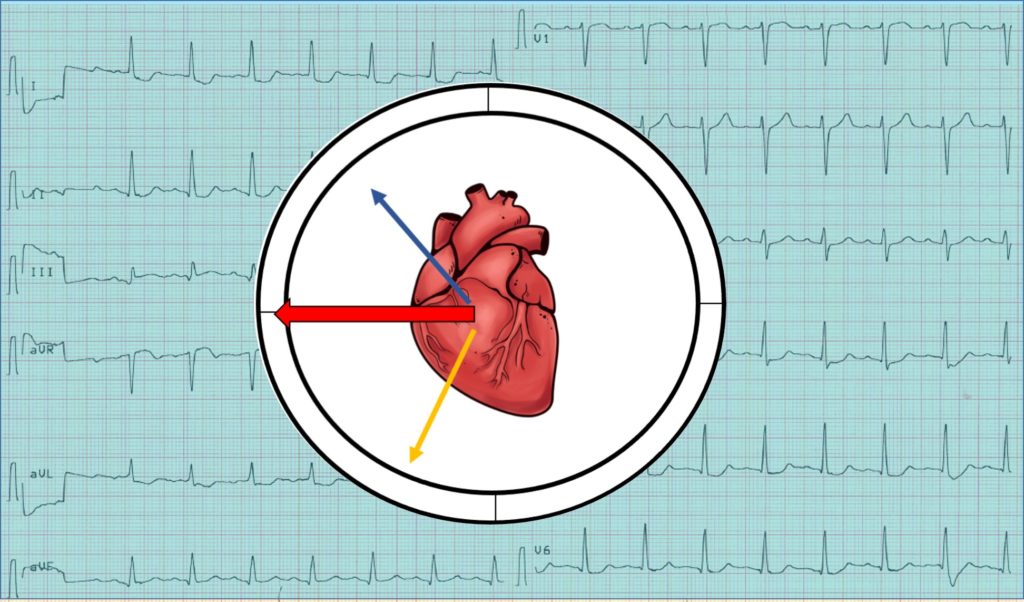
ST vector in Aslanger pattern
In cases of damage to the inferior wall, the ST vector of inferior myocardial infarction localizes the infarction area and is usually directed downward and to the right (orange arrow). In this case, reciprocal changes will be recorded in leads I and aVL.
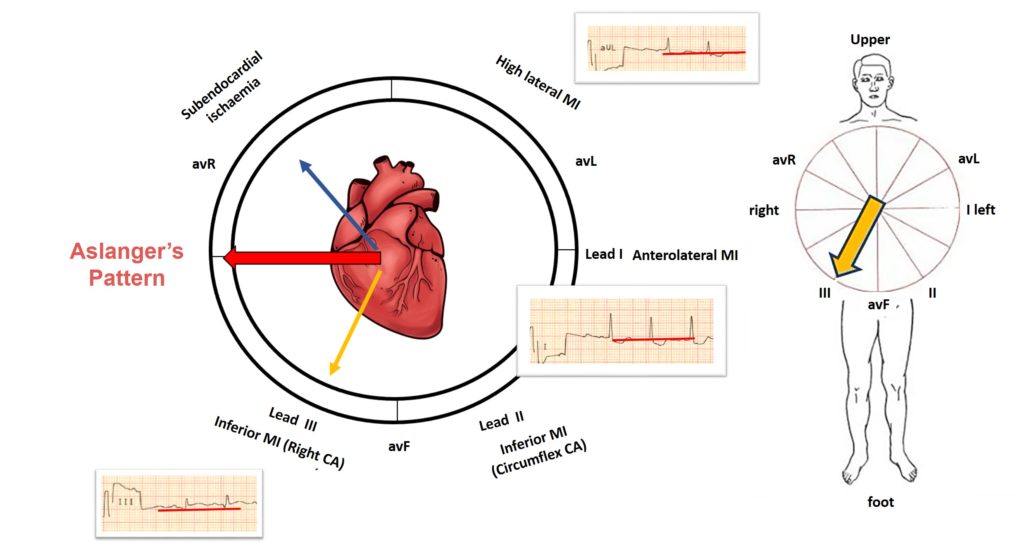
The ST vector of subendocardial ischemia is not localized to ischemia and, regardless of the coronary region affected, indicates lead aVR (blue arrow). The vector of subendocardial ischemia is directed inward from the left heart, towards avR, in which elevation is determined, and in all opposite directions, respectively, depression is visualized.
The resulting middle ST vector is directed to the right, causing ST elevation in lead III and aVR only.
V1 is the rightmost lead on the chest, so ST elevation is also pronounced in V1 in the Aslanger pattern.
Considering that the vector of elevation is directed to the right, therefore, ST-elevation will be more pronounced in V1 than in V2, since lead V1 is to the right than V2.
In addition, mirrored depression to aVR cannot occur in lead V2 because the greater proximity of this lead to aVR compared to other chest leads.
Limitations
It was found that this ECG pattern is also present in 0.5% of patients without acute MI, which may be the result of chronic changes from previous ischemic injury.
Acute inferior myocardial infarction in the presence of previous infarctions can also change the general orientation of the lesion vector, causing a similar picture.
This is an isolated retrospective study that requires further analysis as a predictor of occlusive MI, in which urgent reperfusion therapy is warranted.
Conclusion
Identification of patients with Aslanger’s ECG pattern can facilitate early revascularization and improve the prognosis in this group of patients.
References:
- Aslanger E, Yıldırımtürk Ö, Şimşek B, Sungur A, Türer Cabbar A, Bozbeyoğlu E, Karabay CY, Smith SW, Değertekin M. A new electrocardiographic pattern indicating inferior myocardial infarction. J Electrocardiol. 2020 Jul-Aug;61:41-46.
- Aslanger EK, Smith SW. Response to: “A new electrocardiographic pattern indicating inferior myocardial infarction”. J Electrocardiol. 2020 Nov 18
Register on our website right now to have access to more learning materials!
Acute Pulmonary Edema: Emergency Care Algorithm – Should We Remove or Redistribute the Fluid?
Case Presentation: A 64-year-old man was transported to the emergency department by ambulance due to…
Сounseling a patient with suspected Takotsubo-syndrome OSCE guides
The onset of the consultation Wash hands and put on PPE if necessary. Introduce yourself…
Takotsubo syndrome
Takotsubo syndrome is a condition characterized by the sudden onset of acute, transient (lasting up…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…
Symptomatic bradycardia
Symptomatic bradycardia occurs when the heart rate drops below 50 beats per minute. Most often,…
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…