Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents /OSCE guide

- Opening the consultation
- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role
- Confirm the patient’s name and date of birth
- Explain the reason for the consultation
- Obtain consent for counseling and care
- Availability of a defibrillator
- Provide the availability of a defibrillator
- Start ECG monitoring
- Presenting complaint
- Use open questioning to explore the patient’s presenting complaint
- History of presenting complaint
- Site: ask where the pain is
- Onset: clarify when the pain first started and if it came on suddenly or gradually
- Character: ask the patient to describe how the pain feels
- Radiation: ask if the pain moves anywhere else
- Associated symptoms: ask if there are any other associated symptoms
- Time course: ask how the pain has changed over time
- Exacerbating or relieving factors: ask if anything makes the pain worse or better
- Severity: ask how severe the pain is on a scale of 0-10
- Past medical history
- Screen for conditions that may be associated with chest pain
- Ask about other medical diagnoses and previous surgical history
- Ask if the patient has any allergies and if so, clarify what kind of reaction they had to the substance
- Drug history
- Ask the patient is currently taking any prescribed medications or over-the-counter remedies
- Ask the patient if they’re experiencing any side effects from their medication
- Physical examination
- Assessment of general condition and vital functions according to the ABCDE algorithm
- Visual assessment of the color of the skin, the presence of swelling of the cervical veins, and edema.
- Assessment of the state of the cardiovascular system.
- Assessment of the state of the respiratory system.
- Pulse oximetry to determine blood oxygen saturation (normal ≥ 95%).
- Oxygen therapy (supporting saturation over 94-95%).
- Intravenous access
- Intravenous access
- Starting the infusion of Ringer’s lactate solution
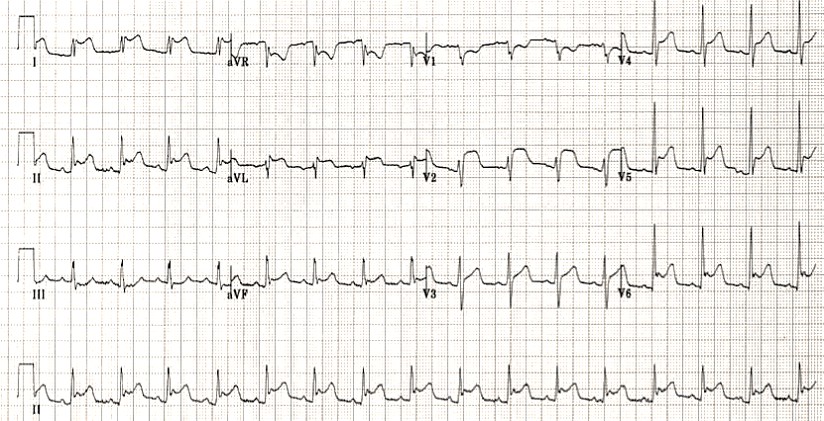
- Registration of a 12-channel ECG
- Recording ECG
- Assess the presence/absence of pathological ST-elevation according to formal STEMI criteria;
- Exclusion of other causes of benign ST-elevation in the presence of such ST-elevation – to exclude a possible non-coronary or acute coronary origin: early ventricular repolarization syndrome, left ventricular aneurysm, secondary ST-changes in LVH, recording artifacts, and others;
- Assessment of additional ECG patterns and conditions that may be caused by critical coronary artery occlusion (STEMI-equivalents) – in the absence of ST-elevation – make sure that there are no other signs of coronary artery occlusion (STEMI equivalents);
- Identification of the localization of myocardial ischemia
- Assess for the presence of right ventricular myocardial infarction
- Express test for the determination of cardiac troponin, myoglobin, creatine phosphokinase-MB, if possible
- The timing of the increase in markers of myocardial damage
- Analysis of other causes that may lead to increased markers of myocardial necrosis
- Making preliminary diagnosis
- Criteria for ACS with ST-segment elevation (STEMI)
- STEMI Equivalents
- Localization
- Killip score
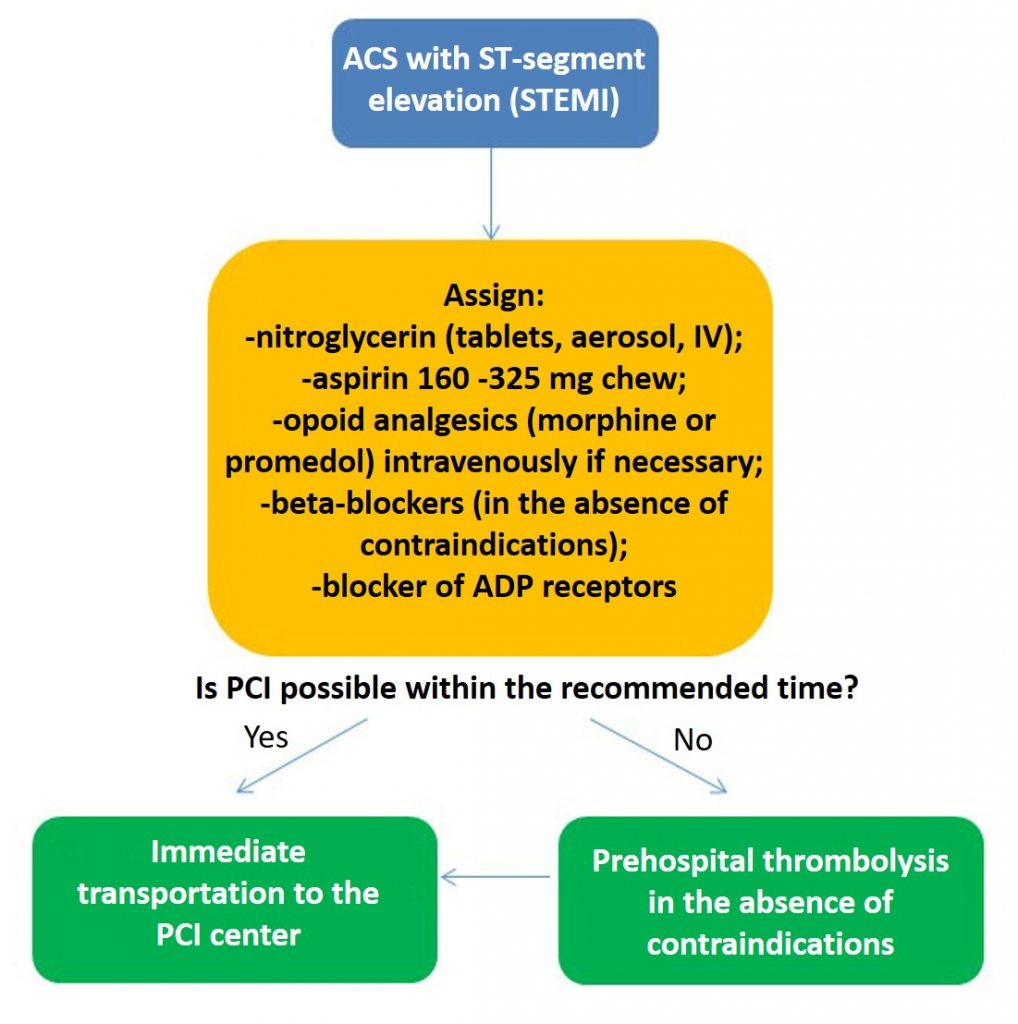
- Drug therapy (basic)
- Acetylsalicylic acid
- Anticoagulant
- Nitroglycerin
- Beta-blocker
- Administering solutions as needed
- Pain relief
- Midozalom administration for cocaine-induced STEMI
- Concomitant therapy as needed
- Evaluation of the door-balloon time (the choice of further reperfusion strategy aimed as soon as possible to restore the coronary blood flow in the infarct-dependent artery)
- Primary PCI
- Hospital thrombolysis followed by PCI
- Call the nearest reperfusion center
- Activation of the intervention team of the reperfusion center
- P2Y12 receptor inhibitor prescription depending on the chosen strategy of reperfusion therapy
- Choice of P2Y12 inhibitor for medical care
- Carrying out thrombolytic therapy as needed
- Criteria for selecting patients for thrombolytic therapy
- Evaluation of success criteria for fibrinolytic therapy
- Choice of the drug for thrombolysis
- Assessment of absolute contraindications for thrombolysis
- Assessment of relative contraindications for thrombolysis
- Transportation to the nearest reperfusion center
- Analysis of delays in the medical care of a patient with acute coronary syndrome
- Monitoring of vital signs during the transfer
- Pain management as needed
- Reporting in the emergency department of the hospital during the patient’s hospitalization
Opening the consultation
- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role
- Confirm the patient’s name and date of birth
- Explain the reason for the consultation
- Obtain consent for counseling and care
Ensure the correct position of the patient, lying with his head slightly raised, to reduce the load on the myocardium, limit physical activity and provide psychological peace.
Confirm the patient’s name and date of birth using the next questions:
| Full | Short |
| “What is your first name?” | “Your first name?” |
| “What is your family name?” “Can you tell me what your family name is?“ | “Your family name?” |
| “Any other names?” | |
| “What`s your date of birth?” | “Your date of birth?“ |
| “When were you admitted?” | “The date you were admitted?” |
| “Can you tell me what your address is?” | |
| “Who is your GP?” |
Availability of a defibrillator
- Provide the availability of a defibrillator
- Start ECG monitoring
When caring for a patient with suspected acute myocardial infarction, a defibrillator should be available to the patient as early as possible, which may be needed for immediate defibrillation if necessary!
As soon as possible, it is necessary to start ECG monitoring, and provide constant monitoring of vital signs.
If the patient is unconscious or unresponsive, start a basic life support (BLS) algorithm in accordance with resuscitation guidelines.
Presenting complaint
Use open questioning to explore the patient’s presenting complaint
- “What’s brought you in to see me today?”
- “What`s brought you along today?“
- “What`s brought you here?“
- “Tell me about the issues you’ve been experiencing.”
- “Can you tell me what seems to be bothering you?”
- “What seems to be the problem?”
- “What can I do for you?“
History of presenting complaint
Take additional information about the patient’s chest pain using the abbreviation SOCRATES. It is important to determine the time of onset of chest pain, its nature, localization, duration, irradiation, the effectiveness of nitroglycerin, provoking factors, comparison of this pain syndrome with previous ones.
SOCRATES
The SOCRATES acronym is a useful tool for exploring each of the patient’s presenting symptoms in more detail. It is most commonly used to explore pain, but it can be applied to other symptoms, although some of the elements of SOCRATES may not be relevant to all symptoms.
- Site: ask where the pain is
- Onset: clarify when the pain first started and if it came on suddenly or gradually
- Character: ask the patient to describe how the pain feels
- Radiation: ask if the pain moves anywhere else
- Associated symptoms: ask if there are any other associated symptoms
- Time course: ask how the pain has changed over time
- Exacerbating or relieving factors: ask if anything makes the pain worse or better
- Severity: ask how severe the pain is on a scale of 0-10
| S | Site | Ask about the location of the pain | • “Where is the pain?” • “Can you point to where you experienced the pain?” • “Can you show me where it hurts?” • ” What body parts are involved?” • “Which part of your (head) is affected?” • “What is the site of the pain?” |
| O | Onset | Clarify how and when the pain developed | • “Did the pain come on suddenly or gradually?” • “When did the pain first start?” • “When did the symptoms start?” • “Did the pain come on at rest or whilst you were exerting yourself?” • “How long did the pain last for?” • “How and when did it start?” • “When did the pain start, and was it sudden or gradual?” • “What were you doing then?” • “Is there anything special that brings on the pain?” • “When does the pain come on?” • “Do you know what contributory causes are cause the attacks?” • “When do the attacks seem to be worse?” |
| C | Character | Ask about the specific characteristics of the pain: | • “How would you describe the pain?” • “Is the pain constant or does it come and go?” • “What is the pain like?” • “Can you describe the pain to me?” • “Is it continuous or does it come and go?” • “What is the character of pain?” • “Is the pain worse now?” • “Is the pain continuous?” |
| R | Radiation | Ask if the pain moves anywhere else | • “Does the pain spread elsewhere?” • “Does the pain go/ radiate/ move anywhere else?” • “Is the pain just in one place or has it moved anywhere else?” • “If the pain is moving to another part of the body, where is this, and is it constant?” • “Is the pain there all the time?” • “In which part of the body has the pain radiated before?” |
| A | Associated symptoms | Ask if there are other symptoms that are associated with the pain | • “Are there any other symptoms that seem associated with the pain?” • “Do you have any other symptoms apart from the pain?” • “Does anything else happen while you have the pain?” • “What other symptoms are present and associated with the pain?” • “Are there any other symptoms?” |
| T | Time course | Clarify how the pain has changed over time | • “How has the pain changed over time?” This question can be useful to determine if the chest pain has become progressively worse over time. An example might be a patient describing chest pain that was initially only present during exertion which is now also present at rest (e.g. unstable angina). • How long have you had this pain? • Does it happen at specific times of the day, or is it constant? • When does the pain occur/start? |
| E | Exacerbating or relieving factors | Ask if anything makes the pain worse or better | • “Does anything make the pain worse?” • “Does anything make the pain better?” • “Does anything change the pain?” |
| S | Severity | Assess the severity of the pain by asking the patient to grade it on a scale of 0-10 | • “On a scale of 0-10, how severe is the pain, if 0 is no pain and 10 is the worst pain you’ve ever experienced?” • How bad is the pain on a scale of 1 to 10? • Can you describe your pain on a scale of 1 to 10? • Is it bad enough to (wake you up)? This allows you to assess the patient’s response to treatments (e.g. pain was initially 8/10 and improved to 3/10 with GTN spray). |
Be polite, use for questions “Can you tell me…?” or “Can you describe…?”
For example:
- “Can you tell me where it hurts?”
- “Can you tell me what your pain is like?”
- “Can you tell me where she works?”
- “Can you tell me what your symptoms are?”
Adjectives for pain
| Aching |
| Scalding/burning |
| Crushing |
| Dull |
| Excruciating |
| Gripping |
| Intense |
| Persistent |
| Piercing/boring |
| Severe |
| Shooting |
| Spasmodic |
| Thunderclap |
| Vague |
Shortness of breath can accompany cardiac pain. For the assessment of shortness of breath ask the patient “Have you had any shortness of breath?“
Typical presentations of chest pain
Acute coronary syndrome:
- Sudden onset central crushing chest pain radiating to the left arm and/or jaw lasting longer than 20 minutes.
- Associated symptoms can include sweating, clamminess, nausea, and shortness of breath.
- Symptoms are often worsened by exertion and improved with GTN spray.
Stable angina:
- Sudden onset central chest pain radiating to the left arm and/or jaw lasting fewer than 20 minutes with complete resolution of pain during rest.
- Often triggered by exertion and resolved with GTN spray and/or rest.
- Associated symptoms include shortness of breath.
Pericarditis:
- Gradual onset of central chest pain worsened by lying flat and improved by leaning forwards.
- Associated symptoms can include fever and fatigue.
Thoracic aortic dissection:
- Sudden onset central chest pain radiating through to the back and is often described as ‘tearing’ in nature.
- Associated symptoms include pre-syncope and syncope secondary to hemodynamic instability.
Pneumonia:
- Gradual onset of sharp chest pain worsened by deep inspiration (pleuritic in nature).
- Associated symptoms include productive cough, shortness of breath, fever, and malaise.
Spontaneous pneumothorax:
- Sudden onset of sharp chest pain worsened by deep inspiration.
- Associated with shortness of breath.
Pulmonary embolism:
- Sudden onset chest pain worsened by deep inspiration (pleuritic in nature).
- Associated symptoms include shortness of breath and hemoptysis (rare).
Gastro-oesophageal reflux:
- Gradual onset central chest pain is typically described as burning in character and worsened by lying flat.
- Associated symptoms can include nausea and vomiting.
Oesophageal spasm:
- Sudden onset central chest pain is relieved by GTN spray (hence it is often confused with acute coronary syndrome).
- Associated symptoms can include dysphagia, heartburn, and regurgitation.
Past medical history
- Screen for conditions that may be associated with chest pain
- Ask about other medical diagnoses and previous surgical history
- Ask if the patient has any allergies and if so, clarify what kind of reaction they had to the substance
Cardiovascular risk factors
When taking a cardiovascular history it’s essential that you identify risk factors for cardiovascular disease as you work through the patient’s history (e.g. past medical history, family history, social history).
Important cardiovascular risk factors include:
- Hypertension
- Hyperlipidemia
- Diabetes
- Family history of cardiac disease
- Smoking
| Ask if the patient has any medical conditions | • “Do you have any medical conditions?” • “Do you have any chronic illnesses?” • “Are you currently seeing a doctor or specialist regularly?” |
| Ask if the patient has previously undergone any surgery (e.g. coronary artery bypass grafts, coronary artery stents, heart valve replacements) | • “Have you ever previously undergone any operations or procedures?” • “When was the operation/procedure and why was it performed?” |
If the patient has a medical condition, you should gather more details to assess how well controlled the disease is and what treatment(s) the patient is receiving. It is also important to ask about any complications associated with the condition including hospital admissions.
Examples of relevant medical conditions
Cardiovascular disease:
- Hypertension
- Hyperlipidemia
- Angina
- Myocardial infarction
- Obesity
- Chronic kidney disease
- Atrial fibrillation
- Stroke
- Peripheral vascular disease
- Rheumatic fever
Respiratory disease:
- Pneumonia
- Pneumothorax
- Pulmonary embolus
Gastrointestinal disease:
- Gastro-oesophageal reflux
- Oesophageal spasm
| Allergies | Questions |
| Ask if the patient has any allergies and if so, clarify what kind of reaction they had to the substance (e.g. mild rash vs anaphylaxis). | • “Do you know if you are allergic to any drugs?” • “What symptoms do you have after taking it?” |
Drug history
- Ask the patient is currently taking any prescribed medications or over-the-counter remedies
- Ask the patient if they’re experiencing any side effects from their medication
| Ask if the patient is currently taking any prescribed medications or over-the-counter remedies | • “Are you currently taking any prescribed medications or over-the-counter treatments?” • “Are you taking any medication at the moment?” • “Do you use any over-the-counter remedies or herbal or homeopathic medicines?” • “How many times a day?” • “Do you always remember to take medicines?“ |
| If the patient is taking prescribed or over-the-counter medications, document the medication name, dose, frequency, form, and route. | |
| Ask the patient if they’re currently experiencing any side effects from their medication | • “Have you noticed any side effects from the medication you currently take?” • “Do you know if you are allergic to any drugs?” • “What symptoms do you have after taking it?” |
Medication examples
Medications commonly prescribed to patients with medical conditions relevant to chest pain:
- Anticoagulants (e.g. pulmonary embolism)
- Antiplatelets (e.g. coronary artery disease)
- Statins (e.g. coronary artery disease)
- Glyceryl trinitrate spray (e.g. angina, oesophageal spasm)
- Calcium channel blockers (e.g. hypertension)
- ACE inhibitors (e.g. hypertension)
- Antibiotics (e.g. pneumonia)
- Colchicine (e.g. pericarditis)
Physical examination
- Assessment of general condition and vital functions according to the ABCDE algorithm
- Visual assessment of the color of the skin, the presence of swelling of the cervical veins, and edema.
- Assessment of the state of the cardiovascular system.
- Assessment of the state of the respiratory system.
- Pulse oximetry to determine blood oxygen saturation (normal ≥ 95%).
- Oxygen therapy (supporting saturation over 94-95%).
Assessment of the general condition and vital functions according to the ABCDE algorithm (A – airway patency, B – breathing, C – blood circulation, D – impaired state of consciousness, E – additional information);
Visual assessment of the color and moisture of the skin, the presence of swelling of the cervical veins, edema;
Assessment of the state of the cardiovascular and respiratory system of the patient.
Check the patient’s respiratory rate:
The normal respiratory rate is 12-20 breaths per minute. Patients with ACS may have tachypnea in an attempt to increase myocardial tissue oxygenation.
Check the patient’s oxygen saturation (SpO2):
The normal SpO2 range is 94-98% in healthy individuals and 88-92% in COPD patients at high risk of CO2 retention.
Hypoxemia may occur due to heart failure and secondary pulmonary edema.
Oxygen therapy at a saturation of 95% is carried out with humidified oxygen using a mask or through a nasal catheter at a rate of 3-5 l/min.
Auscultation of the lung sounds
Wheezing or crepitus on auscultation may be a sign of pulmonary edema due to impaired cardiac function. If the patient is conscious, sit him upright. To increase oxygen saturation, a mask with an oxygen flow rate of 15 liters can be used. If the patient has COPD and a history of CO2 retention, switch to a Venturi mask as soon as possible and properly titrate oxygen.
A decrease in air intake from both sides indicates the need for emergency care.
Pulse
Assess the patient’s pulse:
- Tachycardia is a common sign of ACS.
- Bradycardia is a late sign and often precedes cardiac arrest.
Blood pressure
Assess the patient’s blood pressure:
- Patients may have hypertension due to increased sympathetic activity and pain.
- Hypotension is a late sign and means heart failure.
Auscultation of heart sounds
Identification of pathological heart murmurs.
If the patient has a reduced level of consciousness, review the patient’s medications for drugs that can cause a decrease in the level of consciousness (eg, opioids, sedatives, anxiolytics, insulin, oral hypoglycemic drugs).
Intravenous access
- Intravenous access
- Starting the infusion of Ringer’s lactate solution
Peripheral vein catheterization (providing intravenous access); initiation of Ringer’s lactate solution.
Registration of a 12-channel ECG
- Recording ECG
- Assess the presence/absence of pathological ST-elevation according to formal STEMI criteria;
- Exclusion of other causes of benign ST-elevation in the presence of such ST-elevation – to exclude a possible non-coronary or acute coronary origin: early ventricular repolarization syndrome, left ventricular aneurysm, secondary ST-changes in LVH, recording artifacts, and others;
- Assessment of additional ECG patterns and conditions that may be caused by critical coronary artery occlusion (STEMI-equivalents) – in the absence of ST-elevation – make sure that there are no other signs of coronary artery occlusion (STEMI equivalents);
- Identification of the localization of myocardial ischemia
Assess for the presence of right ventricular myocardial infarction
ECG recording and evaluation must be carried out within at least 8-10 minutes (from first medical contact to diagnosis)!
ECG recording should not be given priority over providing emergency care if necessary (resuscitation)!
After the ECG recording an assessment should made of the presence of ST segment elevation and other ECG patterns associated with critical occlusion of the coronary arteries.
Pathological ST segment elevation is considered:
- new ST segment elevation in two consecutive limb leads ≥0.1 mV (≥1 mm)
- elevation
- ≥0.2 mV in men ≥40 years old, ≥0.25 mV in men <40 years old in leads V2-V3,
- ≥1.5 mV in women (≥ 1.5 mm) in leads V2-V3.
- In patients with inferior wall myocardial infarction (ST-segment elevation in II, III, AVF), it is recommended to record the right precordial leads (V3R and V4R) to exclude ST-segment elevation, which indicates right ventricular myocardial infarction.
In patients with inferior wall myocardial infarction (ST-segment elevation in II, III, AVF), it is recommended to record the right precordial leads (V3R and V4R) to exclude ST-segment elevation, which indicates right ventricular myocardial infarction.
When evaluating elevation, if there is elevation in II, III, avF leads, and if there is elevation in V4R, do not prescribe nitroglycerin!
If ST segment depression is detected in leads V1-V3, additionally take an ECG in V7-V9
Signs of acute ischemia against the background of chronic blockade of the left bundle branch block or in the presence of an artificial pacemaker::
- the presence of ST segment elevation of more than 1 mm in the taps with a positive deviation of the QRS complex,
- the presence of ST-segment elevation of more than 5 mm in the leads with a negative deviation of the QRS complex.
Patients with STEMI usually have acute chest pain and sustained (>20 minutes) ST-segment elevation.
ST-elevation is a sign of complete occlusion of the epicardial coronary artery by a thrombus, which causes immediate myocardial death in the affected area of the myocardium::
- Anterior: V1-V4
- Lower: II, III, aVF
- High lateral: I, aVL
- Low lateral: V5, V6
- Posterior: dominant R wave in V1-3 with ST depression in V1-3 (mirror image of anterior MI)
In the absence of characteristic ECG signs against the background of clinical manifestations of ACS, it is necessary to repeat the ECG registration with an interval of 20-30 minutes, paying attention to the presence of sharp T waves, which may precede ST segment elevation;
Once the electrodes are positioned and the wires are properly attached, the patient should be covered with a sheet for moral purposes.
However, traditional STEMI criteria often fail us, as more than 30% of cases of acute coronary occlusion are misclassified and interpreted. In addition, the STEMI/NSTEMI paradigm depends on ST elevation as defined by millimeter criteria, however, many occlusive myocardial infarctions (OMIs) do not have ST elevation at all.
In the current paradigm of STEMI and NSTEMI, 25–30% of patients with STEMI have an unrecognized acute total occlusion (OMI) on delayed angiography (24 hours after symptom onset) and is twice as high in patients with STEMI without OMI (MI without occlusion or NOMI). Conversely, 15–35% of catheter labs are activated through probable STEMI criteria that are false positive and unsupported by angiographic assessments of causative coronary artery disease.
«NSTEMI» – 25% false negative (skipping occlusions with 2x mortality)
«STEMI» – 15-35% false positive (iatrogenic harm and waste of resources)
Assessment of additional ECG patterns and conditions that may be accompanied by critical coronary artery occlusion
ECG signs suggestive of coronary artery occlusion in the absence of ST-elevation have long been known. They are called “STEMI equivalents”:
- LBBB combined with Sgarbosa’s original/modified criteria
- Posterior MI
- ST-elevation in aVR
- Pattern De Winter
- Wellens Syndrome
- Sharp T waves
- Pacemaker rhythm combined with Sgarbosa’s original/modified criteria
It is also known that so-called benign (non-ischemic) ST-elevation can occur, for example:
- syndrome of early repolarization of the ventricles;
- recording artifacts simulating ST segment elevation;
- secondary ST changes against the background of LV myocardial hypertrophy, LBBB;
- imitation of ST deviations due to the superimposition of waves of atrial fibrillation/trembling, etc.
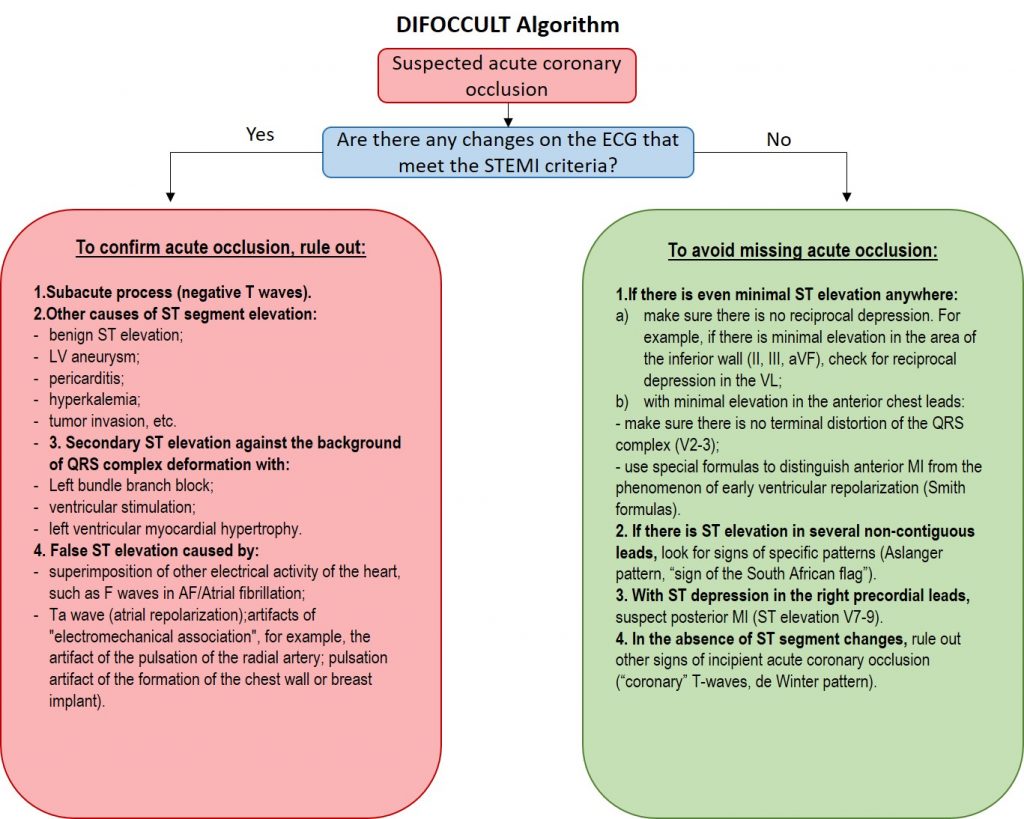
The algorithm for differential diagnosis depends on the presence (Table 2.) or absence of ST segment elevation (Table 3.), which meets the STEMI criteria.
Table 2. ST-elevation meeting STEMI criteria
| ST-segment elevation meeting STEMI criteria | |
| Step 1 – Artifact Exclusion. You should make sure that the ST-segment elevation does not have an artifactual appearance. | – Atrial activity – Electromechanical Association – ECG filtering |
| Step 2 – Exclusion of depolarization disorders. Secondary ST elevation should be ruled out in case of impaired depolarization. It is necessary to determine if the QRS complex is wide. If so, then secondary ST-T wave deviations are expected even without OMI. In these situations, the ST deviation is in a direction that is opposite to the direction of the main QRS vector, and it is proportional to the amplitude of the QRS complex, called the “corresponding dissonance”. | – Blockade of the left leg of the bundle of His – Ventricular pacing rhythm – Blockade of the right leg of the bundle of His – Wolff-Parkinson-White Syndrome – Hyperkalemia |
| Step 3 – Rule out other causes of secondary ST elevation. Rule out other causes of secondary ST-elevation. If the QRS duration is normal but the amplitude or configuration is abnormal, then there may be an abnormality that affects both depolarization and repolarization. | – Left ventricular hypertrophy – Use ST/T ≥1/6 to detect OMI. – Persistent ST elevation – Use T/QRS ≥1/3 to detect OMI. |
| Step 4 – Rule out other causes of primary ST-elevation. | – Pericarditis (ST-depression aVL Terminal QRS distortion) – Early repolarization (ST depression aVL Terminal QRS distortion) – Other reasons: – Myocarditis – Takotsubo cardiomyopathy – Brugada Syndrome – Massive pulmonary embolism – Tumor growth |
| Step 5 – Presence of ST-elevation, but with T-wave inversion. ST-elevation may persist in a patient with pain relief after spontaneous reperfusion or in a subacute process. | ST-elevation combined with negative T wave. – Subacute myocardial infarction – Wellens Pattern |
Table 3. Absence of ST-elevation that meets STEMI criteria
| No ST-segment elevation that meets STEMI criteria | |
| Step 6 – Recognize Certain Patterns with Single Lead ST Elevation Only | – Aslanger Pattern – Sign of the South African flag on the ECG |
| Step 7 – Look carefully at the ECG to look for slight ST-elevation | – Minimal reciprocal changes — Explore pairs of opposite leads — Use formulas for differential diagnosis of benign ST segment elevation and OMI |
| Step 8 – If there is no ST-elevation, look for ST-depression | “Posterior” myocardial infarction De Winter pattern |
| Step 9 – Look for sharp T waves | |
| Step 10 – Check everything again |
A complex display of the discussed algorithm is presented in the images:

Therefore, ECG data can recognize coronary occlusion without ST-segment elevation (“STEMI equivalents”), and also be able to distinguish ST-elevation in acute coronary occlusion from elevation due to other causes (early ventricular repolarization syndrome, ST artifacts, subacute stage acute myocardial infarction, that is, with conditions that do not require thrombolysis or emergency coronary angiography.
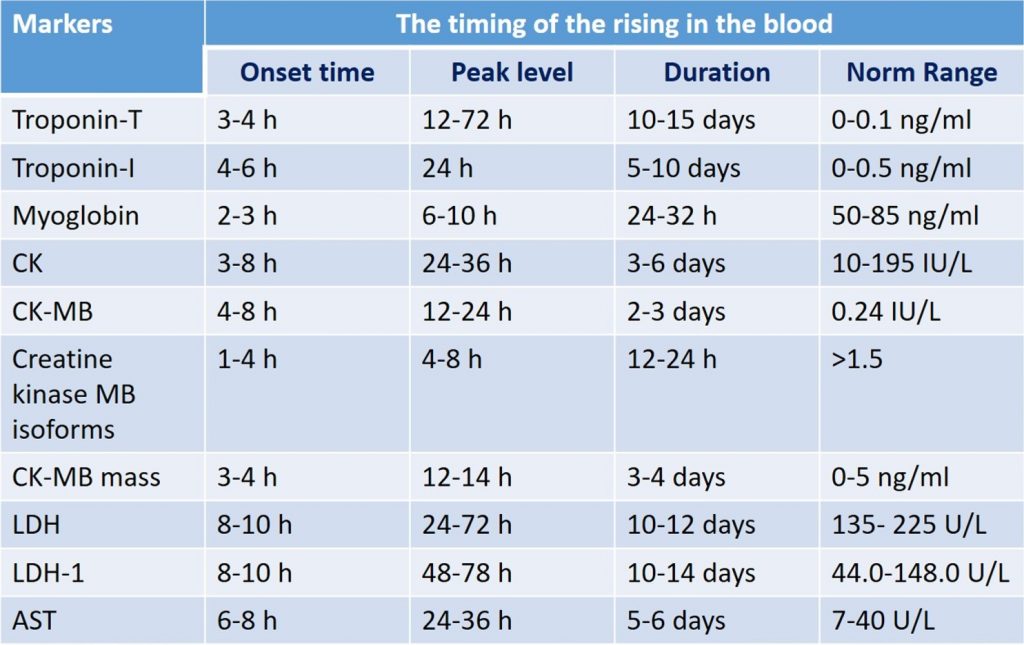
Express test for the determination of cardiac troponin, myoglobin, creatine phosphokinase-MB, if possible
- The timing of the increase in markers of myocardial damage
- Analysis of other causes that may lead to increased markers of myocardial necrosis
The timing of the increase in markers of myocardial necrosis is presented in the table. It should be noted that the levels of Myoglobin and creatine phosphokinase, the creatine phosphokinase-MB (CPK-MB) isoform, are the first to increase.
Other causes of increased markers of myocardial necrosis
There are many causes of elevated troponin levels, including:
- Myocardial infarction
- Tachy/bradyarrhythmias
- Aortic dissection
- Severe aortic valve disease
- Hypertrophic cardiomyopathy
- Severe respiratory failure
- Severe anemia
- Coronary spasm
- Heart failure
- Takotsubo cardiomyopathy
- Sepsis
- Kidney failure
- Stroke
- Subarachnoid hemorrhage
Preliminary diagnosis
- Criteria for ACS with ST-segment elevation (STEMI)
- STEMI Equivalents
- Localization
- Killip score
Classification of acute heart failure Killip
| Class I | No sign of congestion |
| Class II | S3 and basal rales on auscultation |
| Class III | Acute pulmonary edema |
| Class IV | Cardiogenic shock |
Interpretation:
| Class | 30-day mortality * | In-hospital mortality** (historical interest only) |
| I | 2-3% | <6% |
| II | 5-12% | <17% |
| III | 10-20% | 38% |
| IV | 10-20% | 81% |
* From Khot 2003 who combined class III/IV due to the relatively smaller number of patients in class IV (0.3% of patients).
** From Killip 1967. This classification was developed as early as the 1960s, before being introduced into the clinical practice of reperfusion therapy (thrombolytics, PCI); however, since then, several studies have shown that the Killip classification still predicts mortality for both STEMI and NSTEMI. However, there is certainly a significant decrease in mortality compared to the original study.
Drug therapy (basic)
- Acetylsalicylic acid
- Anticoagulant
- Nitroglycerin
- Beta-blocker
- Administering solutions as needed
- Pain relief
- Midozalom administration for cocaine-induced STEMI
- Concomitant therapy as needed
| Acetylsalicylic acid | Acetylsalicylic acid – 324 mg chew (81 mg / tab. x 4) or 325 mg without enteric coating (if the patient did not take it before the arrival of the ambulance team), use a non-enteric form. In the presence of contraindications to ASA, it is possible to use clopidogrel at a dose of 300 mg orally. |
| Anticoagulant | Heparin 60 units/kg IV, maximum dose 4000-5000 units. |
| Nitroglycerin | – Nitroglycerin 0.4 mg sublingually (if SBP is more than 110 mm Hg intravenous, if more than 120 mm Hg, tablet intake without intravenous administration). – Nitroglycerin can be repeated three times if symptoms persist, pain does not improve, every five minutes, and BP values are above 90 mmHg and pulse over 60 beats per minute up to a maximum dose of 1.2 mg. If blood pressure drops by 20 mm Hg after the use of nitroglycerin, the subsequent intake of nitroglycerin should be coordinated. – In the presence of severe pain syndrome, an IV infusion of 2.0 ml of 1% nitroglycerin, previously dissolved in 200 ml of 0.9% sodium chloride solution or 5% dextrose solution, is possible under close control of blood pressure and heart rate at an initial rate of 5 μg / min, which can be increased every 3-5 minutes by 5 mcg/min. If a therapeutic effect is not obtained at an injection rate of 20 μg / min, a further increase in the rate of administration should be 10-20 μg / min. As a rule, to achieve the effect, the rate of administration of nitroglycerin is not more than 100 mcg/min. If during the infusion of nitroglycerin, systolic blood pressure becomes ˂ 90 mm Hg (or mean blood pressure decreases by 10-25% of baseline), the infusion should be stopped. – Nitroglycerin should be avoided – in patients with erectile dysfunction taking Viagra (Sildenafil), Levitra (Vardenafil), Ciais (Tadalafil), as well as in patients with pulmonary hypertension taking Adcirca (Tadalafil), Revacio, also epoprostenol or trepostenil, if indicated drugs have been used within the last 48 hours. – Avoid using nitrates if right ventricular infarction is suspected! |
| Beta-blocker | Beta-blocker metoprolol 5 mg is intravenous for hypertension or tachycardia. Administer as early as possible to all patients with ACS without contraindications to their use (bradycardia, clinical signs of hypotension or congestive heart failure, pulmonary edema, blockade, asthma/COPD, cocaine use, ST-elevation in II, III, aVF)! Propranolol and esmolol can also be used. |
| Introduction of solutions | If there is a myocardial infarction of the lower wall, with an elevation of ST II, III, avF, it is necessary to start the introduction of solutions |
| Pain management | If chest pain persists, consider fentanyl 25-100 mg. If fentanyl is not available, consider morphine, and if pain persists, opioid morphine 2–5 mg every 5–15 minutes is recommended until pain and dyspnoea resolve or side effects (hypotension, respiratory depression, nausea, vomiting) occur. |
| Cocaine-induced STEMI | If cocaine-induced STEMI has been reported, midazolam 2.5 mg IV or 5 mg PO if midazolam is not available, consider lorazepam. |
| Concomitant therapy if necessary | If there is vomiting, nausea, ondansetron 4 mg IV or IM or 8 mg orally in tablets. |
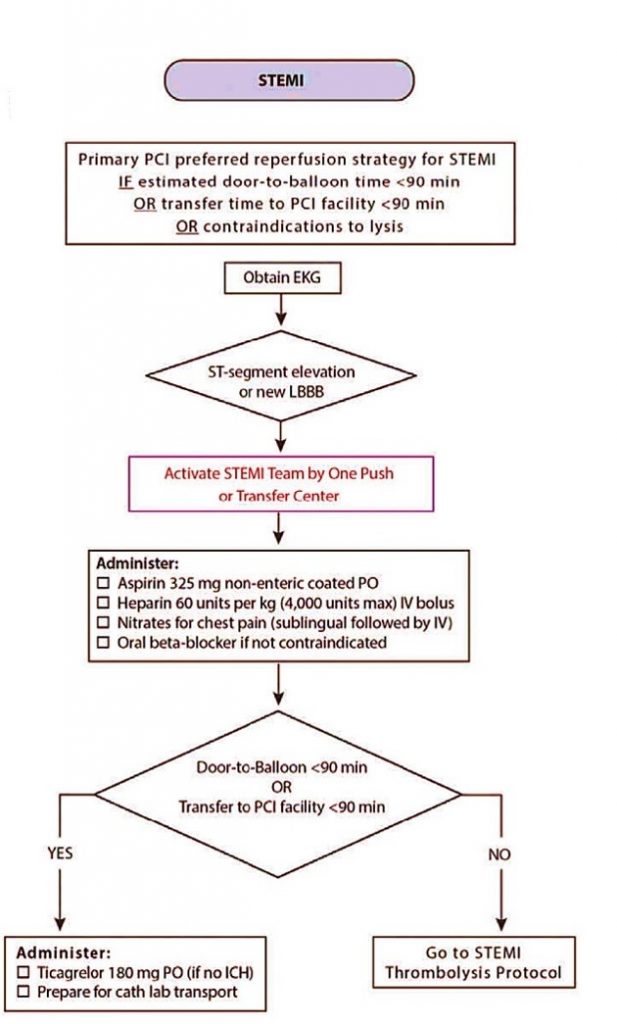
Evaluation of the door-balloon time (the choice of further reperfusion strategy aimed as soon as possible to restore the coronary blood flow in the infarct-dependent artery)
- Primary PCI
- Hospital thrombolysis followed by PCI
Evaluation of the door-balloon time (the choice of further reperfusion strategy aimed as soon as possible to restore the coronary blood flow in the infarct-dependent artery)
- Primary PCI
- Hospital thrombolysis followed by PCI
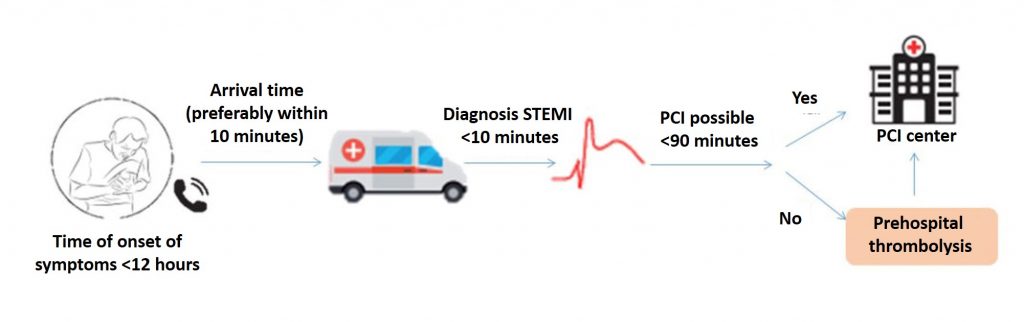
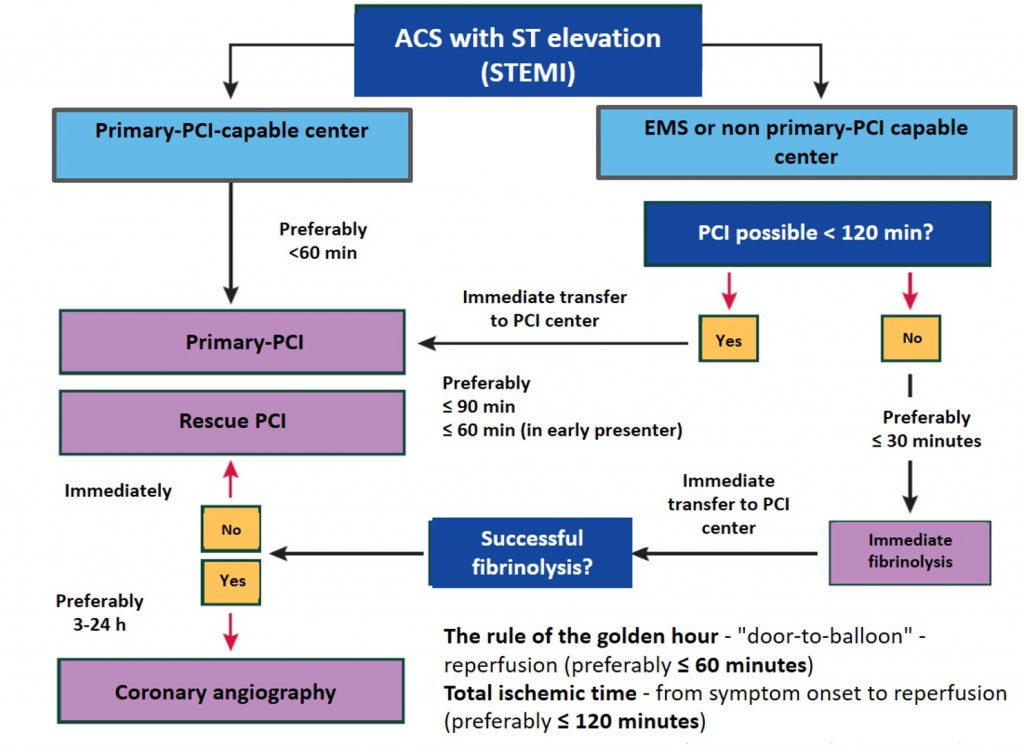
If the criteria for ACS are met, the patient should be taken to the nearest reperfusion center as soon as possible!
When providing medical care to a patient with acute coronary syndrome with ST-segment elevation or its equivalent, the distance to the center of percutaneous coronary intervention is assessed.
| Balloon door time estimate (less than 120 minutes, preferably less than 90-60 minutes) | Balloon door time estimate (more than 90-120 minutes) |
| If the estimated balloon door time is less than 120 minutes, preferably less than 90-60 minutes, or transfer to a percutaneous coronary intervention center less than 90 minutes, then thrombolysis is not performed and the patient is transported to a primary PCI center. The patient should be given ticagrelor 180 mg and prepared for transport to the catheter laboratory at the percutaneous coronary intervention center. | If it is not possible to perform primary PCI within 120 minutes or transfer to a percutaneous coronary intervention center for more than 90 minutes, consider thrombolysis. Thrombolysis must be performed within 30 minutes of the primary medical contact and the patient transported to the primary PCI center. |
The optimal method of reperfusion therapy for ACS with ST-segment elevation is percutaneous coronary intervention (PCI). Primary PCI should be performed as early as possible, preferably within 60-90 minutes (in high-risk cases in patients with large anterior myocardial infarction, preferably no later than 60 minutes). If it is impossible to transport the patient to the PCI center within 60-90 minutes, pre-hospital thrombolysis is recommended in the absence of contraindications.
If the time from the onset of pain is less than 90 minutes and the time to transport the patient to the center is <120 minutes, the patient should be immediately transported to the PCI center without prior thrombolysis.
Scheme of patient with STEMI transportation (ACS with ST-segment elevation)
Algorithm for providing assistance at the prehospital stage
- An initial PCI is warranted within the first 3-24 hours.
- Don’t forget the golden hour rule.
- Reperfusion of the balloon door is desirable in less than 60 minutes.
- Total ischemic time – the time from symptom onset to reperfusion – preferably less than 120 minutes.
Call the nearest reperfusion center
- Activation of the intervention team of the reperfusion center
If the patient meets STEMI criteria or STEMI equivalents, then the patient is a priority patient requiring immediate notification to the nearest reperfusion heart center to allow the hospital to prepare.
In some countries, there is a verbal statement called “STEMI ALERT” indicating that the patient meets the criteria for acute coronary syndrome with ST-segment elevation (STEMI).
Based on the report of the emergency doctor, the doctor on the duty at the hospital, who is also responsible for communication with the emergency medical service, informs and activates the team of interventional cardiologists.
What you need to mention during the phone conversation – key points for communication::
- Patient priority
- Age
- Presenting complaint
- Impressions of the emergency medical care /Paramedic
- Characteristic signs and symptoms in the patient (eg HR, respiratory rate, BP, oxygen saturation)
- Do not mention if recorded values are within normal limits or if the patient is stable
- Duration of symptoms
- 12-channel ECG interpretation
- Relevant physician findings
P2Y12 receptor inhibitor prescription depending on the chosen strategy of reperfusion therapy
- Choice of P2Y12 inhibitor for medical care
P2Y12 receptor inhibitors: pharmacological properties
| Property | Clopidogrel | Рrasugrel | Ticagrelor |
| Receptor blockade | Irreversible | Irreversible | Negotiable |
| Prodrugs | Yes | Yes | No |
| Half-life | About 6 hours | About 7 hours | 8-12 hours |
| Binding type | Competitive | Competitive | Non-competitive |
| Administration | Oral | Oral | Oral |
| Dosing frequency | 1 per day | 1 per day | 2 times a day |
| Effect start | 2-8 hours | From 30 min to 4 hours | From 30 min to 4 hours |
| End of the effect | 5-7 days | 7-10 days | 3-5 days |
| Interaction of the drug with enzymes of the cytochrome system | CYP2C19 | No | CYP3A |
| Approved readings | ACS (invasive or non-invasive treatment) and PCI for stable CAD | PCI in patients with ACS | ACS (invasive or non-invasive therapy (excluding thrombolytic therapy)) |
The use of P2Y12 antagonists in acute coronary syndrome (ACS) has potential advantages: reduction in the incidence of intraprocedural and postprocedural stent thrombosis, and reduction of periprocedural myocardial infarction.
Clopidogrel, prasugrel, or ticagrelor are the most commonly used P2Y12 receptor antagonists.
Clopidogrel is an irreversible P2Y12 receptor antagonist. The onset of action is dose-dependent (loading dose 600 mg versus loading dose 300 mg) with onset 2-6 hours later. This dynamic makes clopidogrel less effective in preventing stent thrombosis before PCI.
Prasugrel is another irreversible oral P2Y12 antagonist. Its onset of action is faster compared to clopidogrel (30 minutes – 4 hours versus 2-6 hours).
Ticagrelor is a reversible oral P2Y12 antagonist that, unlike clopidogrel and prasugrel, does not require in vivo conversion to an active metabolite.
Therefore, the onset of action is much faster (30 minutes – 2 hours). Ticagrelor has been approved for use in patients with ACS (both NSTEMI and STEMI).
Loading dosage of ticagrelor 180 mg.
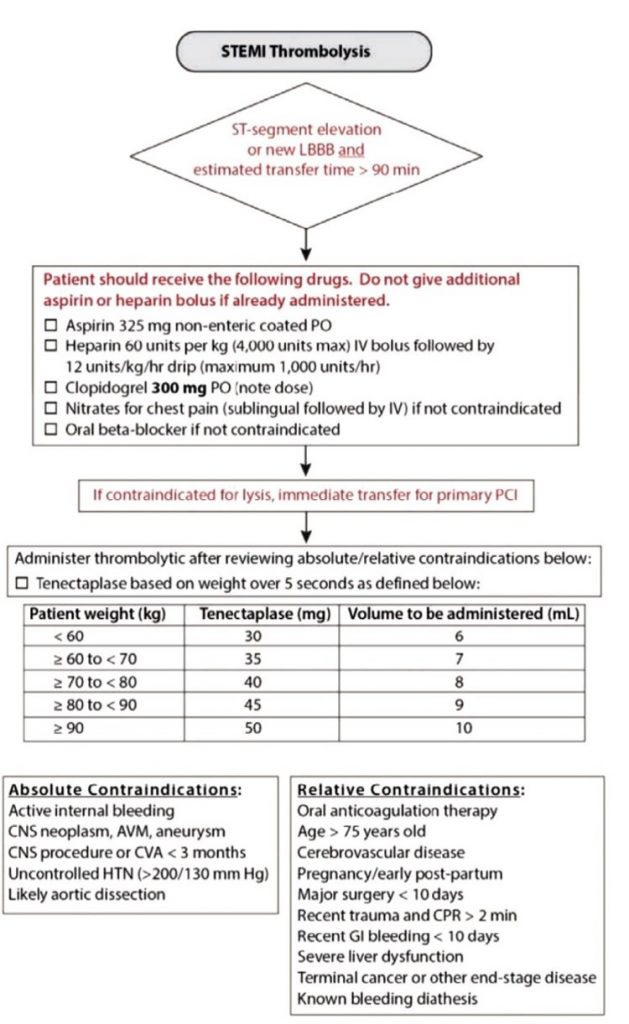
Carrying out thrombolytic therapy as needed
- Criteria for selecting patients for thrombolytic therapy
- Evaluation of success criteria for fibrinolytic therapy
- Choice of the drug for thrombolysis
- Assessment of absolute contraindications for thrombolysis
- Assessment of relative contraindications for thrombolysis
Prehospital thrombolysis
Criteria for selecting patients for thrombolytic therapy:
- diagnosis of STEMI (ACS with ST-segment elevation);
- symptoms onset 12 hours;
- lack of opportunities for providing PCI within up to 90 minutes from the first medical contact with the patient to the introduction of the balloon;
- absence of contraindications to thrombolysis;
- availability of informed consent of the patient.
An important criterion for the success of fibrinolytic therapy is the reduction of ST-segment elevation by at least 50% within 60-90 minutes from the start of fibrinolytic administration.
Before the introduction of streptokinase and alteplase, a bolus of heparin 5000 IU IV is recommended.
If fibrinolytic therapy is necessary, preference is given to fibrin-specific drugs.
| Drug | Dosage |
| Streptokinase | 1.5 million IU for 30-60 minutes IV drip |
| Alteplase | 15 mg IV bolus, then 0.75 mg/kg (maximum 50 mg) IV over 30 minutes, then 0.5 mg/kg (maximum 35 mg) IV for the following 60 minutes |
| Tenecteplase | Single IV bolus: 30 mg (6000 IU) with a weight of 60 kg; 35 mg (7000 IU) with a weight of 60-70 kg; 40 mg (8000 IU) with a weight of 70-80 kg; 45 mg (9000 IU) with a weight of 80-90 kg; 50 mg (10,000 IU) for weight ≥90 kg. For patients ≥75 years of age, a dose reduced by half is recommended. |
Contraindications for thrombolysis:
| Absolute contraindications: | Relative contraindications: |
| – intracerebral hemorrhage or hemorrhagic stroke of any prescription; – ischemic stroke during the previous 6 months; – trauma to the central nervous system or tumor of the central nervous system or a known arteriovenous malformation; – recent major trauma/surgery/head injury within the previous month; – gastrointestinal bleeding during the previous month; – established blood disease, accompanied by bleeding; – active bleeding (except menstruation); – dissecting aortic aneurysm; – punctures in places that cannot be squeezed by applying a compression bandage performed within the previous 24 hours (for example, liver biopsy, lumbar puncture). | – transient ischemic attack within the previous 6 months; – concomitant oral anticoagulant therapy; – pregnancy or 1 week after childbirth; – refractory hypertension (SBP ˃180 mm Hg and/or DBP ˃110 mm Hg); – severe liver disease; – infective endocarditis; – active peptic ulcer; – prolonged (2 min) or traumatic resuscitation. |
It is necessary in the first 24 hours from the onset of symptoms of myocardial infarction to transfer the patient after fibrinolytic therapy to the hospital with PCI opportunities.
Transportation to the nearest reperfusion center
- Analysis of delays in the medical care of a patient with acute coronary syndrome
- Monitoring of vital signs during the transfer
- Pain management as needed
- Reporting in the emergency department of the hospital during the patient’s hospitalization
A generalized algorithm for transporting a patient with ST-segment elevation ACS is presented below.
Note: EMS – emergency medical service, PCI – percutaneous coronary intervention
Every patient with ACS with ST-segment elevation after receiving emergency care at the prehospital stage should be immediately admitted to the hospital.
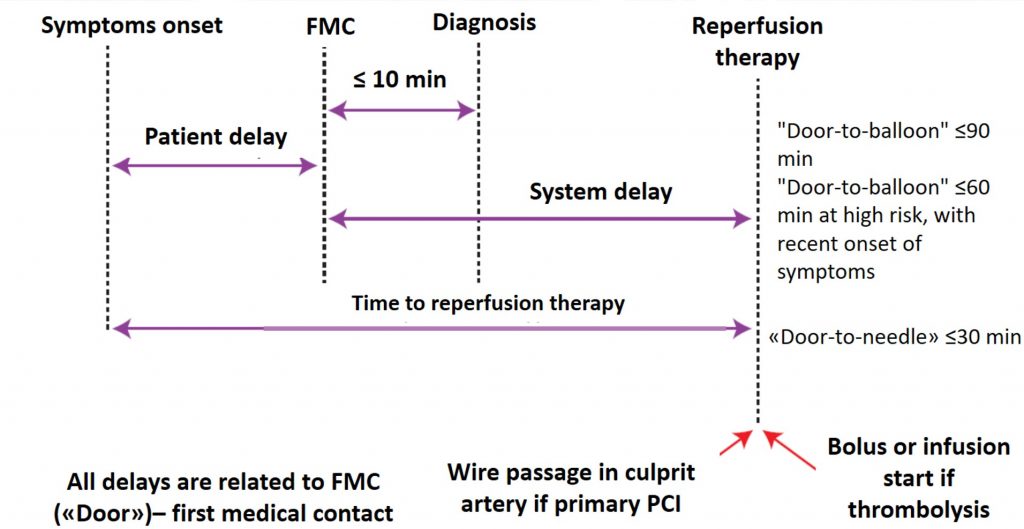
At the same time, hospitalization in a healthcare facility with the possibility of emergency percutaneous coronary intervention (PCI) is an absolute priority. Unfortunately, this possibility is not always available, and sometimes patients are admitted to healthcare facilities without this possibility.
When transporting patients, it is recommended to carefully monitor all vital signs, and, most importantly, to record a series of ECGs – preferably every 15 minutes (rather than an hour or two), if possible, perform a troponin test. Hospital physicians should be notified that the arrival of such a patient is being prepared so that they can activate the entire reperfusion center team and prepare the catheter laboratory for intervention. When hospitalized in a hospital, it is necessary to continue to record ECG series and evaluate troponin in dynamics, if possible, perform an Echo-ECG.
In the management of the patient with ST-segment elevation, delay reduction is critical, as early reperfusion is critical and has been proven to improve the prognosis of these patients.
- Patient delay – the delay between the onset of symptoms and the initial medical contact.
- The delay between initial medical contact and diagnosis – is the time required to record the first ECG. The goal should be to get this delay down to 10 minutes or less – preferably 8 minutes.
- System delay – the delay between the initial medical contact and reperfusion therapy (initial medical contact before the guidewire is inserted into the infarct-dependent artery).
- If the reperfusion strategy has chosen primary percutaneous intervention, then the goal should be to reduce system delay to ≤90 min, and in high-risk cases with large anterior infarction and symptoms within 2 hours, this time should be reduced to less than 60 min).
- If reperfusion therapy is fibrinolysis, the goal is to reduce this delay (primary medical contact to the needle) to ≤30 min.
- Total ischemic time. From the patient’s point of view, the delay between the onset of symptoms and the provision of reperfusion therapy (either onset of fibrinolysis, or insertion of a guidewire into an infarct-dependent artery) is a total ischemic time that should be minimized as much as possible (preferably less than 120 minutes).
The graphic scheme of time delays is shown in the figure:
When reporting in relation to the patient to the duty cardiologist of the emergency medical center in the emergency department of the hospital during the patient’s hospitalization:
- Complaints of the patient;
- Data of the physical examination at the time of FMC and during transportation;
- Identified ECG changes;
- Provision of ECG archives recorded during FMC and transportation of the patient to the hospital;
- Amount of care provided and patient response to the treatment;
- Provision of relevant records of the patient’s medical history.
Additional materials:
Literature:
- 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal (2018) 39 (2), 119-177. doi:10.1093/eurheartj/ehx393.
- 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal, V.39, Issue 3, 14 January 2018, Pages 213-260, https://doi.org/10.1093/eurheartj/ehx419.
- Continuum of care for acute coronary syndrome: optimizing treatment for ST-elevation myocardial infarction and non-elevation acute coronary syndrome. W. Brian Gibler, Judy M. Racadio et al. EMCREG-International Monograph February. Critical Pathways in Cardiology (2018), V.17, №3.
- 2019 ESC/EAS Guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. European Heart Journal, Volume 41, Issue 1, January 2020,p. 111-188. doi: 10.1093/eurheartj/enz455.
- 1. Meyers HP, Bracey A, Lee D, Lichtenheld A, Li WJ, Singer DD, Kane JA, Dodd KW, Meyers KE, Thode HC, Shroff GR, Singer AJ, Smith SW. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. J Emerg Med. 2021 Mar;60(3):273-284. doi: 10.1016/j.jemermed.2020.10.026. Epub 2020 Dec 9. PMID: 33308915.
- Meyers PH, Weingart S, Smith SW. The OMI Manifesto. Dr Smith’s ECG blog 2018
- Alblaihed L. The DIFOCCULT Trial: Time to Change from STEMI/NSTEMI to OMI/NOMI? REBEL EM
- H. Pendell Meyers, Alexander Bracey, Daniel Lee, Andrew Lichtenheld, Wei J. Li, Daniel D. Singer, Zach Rollins, Jesse A. Kane, Kenneth W. Dodd, Kristen E. Meyers, Gautam R. Shroff, Adam J. Singer, Stephen W. Smith, Accuracy of OMI ECG findings versus STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction, IJC Heart & Vasculature, Volume 33, 2021, 100767, https://doi.org/10.1016/j.ijcha.2021.100767
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
SAVED VTE Score
SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators.