Arrhythmogenic cardiomyopathy

Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a hereditary cardiac disorder characterized by fibro-fatty replacement of the right ventricular myocardium, and a predilection to potentially fatal ventricular arrhythmias. The disorder may progress to right ventricular dilatation and failure. Recent researches describe this cardiomyopathy as biventricular, in most cases, also admitting the possibility of a prevalent or exclusive involvement of the LV, known as ‘Left-Dominant’ variant.
Aetiology
The transmission is mostly autosomal dominant. Less frequently the transmission is autosomal recessive and associated with palmoplantar keratoderma and woolly hair (Naxos and Carvajal syndromes).
Currently 16 genes, whose mutations are responsible for the disease, have been identified. The most frequently detected pathogenetic mutations affect 5 genes encoding for desmosomes, structures involved in cell-to-cell adhesion.
Epidemiology
- The prevalence is reported as between 1 in 2000 and 1 in 5000.
- Males are most affected, with a 3:1 ratio.
- The onset of disease occurs at young age, between the second and fourth decade; it is one of the main causes of SCD in young adults and athletes.
- First-degree family members could be mutation carriers, therefore a clinical screening with ECG and echocardiogram starting from 10 to 12 years of age is recommended and, even if negative, must be repeated with individualized timing of re-evaluation.
Pathophysiology
Macroscopically, the typical structural changes in ARVC include RV dilatation with associated RV myocardial thinning and fibro-fatty infiltration; the focal fibro-fatty deposits are the arrhythmogenic substrate that is a hallmark of ARVC.
Left ventricular involvement can be a late feature or an isolated form of the disease.
Particular sites involved include the RV apex, inflow tract, and outflow tract. With disease progression, further involvement of the RV free wall leads to aneurysms and RV cavity dilatation.
Symptoms
Patients are often asymptomatic, but symptoms of palpitations, pre-syncope and syncope can occur and may be precipitated by exercise.
Ventricular arrhythmias (i.e. premature ventricular contractions, non-sustained ventricular tachycardia) can occur, together with major and potentially fatal arrhythmias, also during exercise.
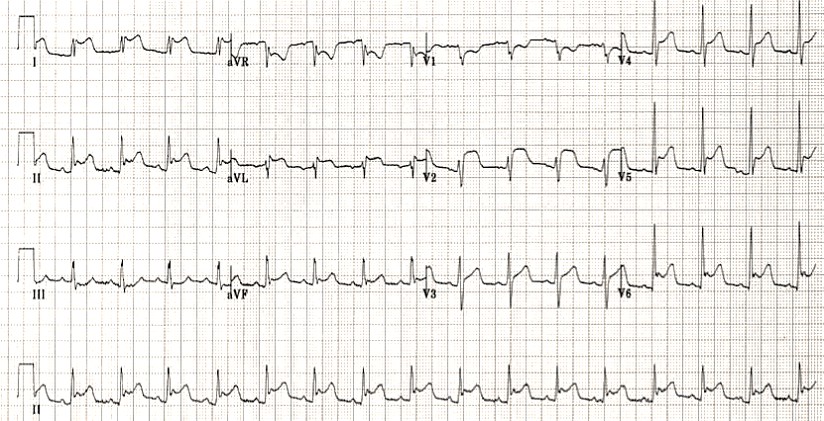
The most typical arrhythmias in ARVC have a left bundle branch block morphology, with negative QRS in the right precordial leads and vertical axis on the frontal plane.
The natural history of ARVC may be separated into a number of distinct phases with progressive development of symptoms and structural abnormalities:
- concealed phase: a subclinical asymptomatic phase with little or no structural RV abnormality. Sudden CD may still occur in this stage of disease;
- overt electrical disorder: typically, with symptomatic ventricular arrhythmias of RV origin. Arrhythmia may vary from premature ventricular beats to non-sustained ventricular tachycardia to ventricular fibrillation. Structurally, there is clear evidence of RV wall involvement;
- RV failure: progressive loss of RV myocardium due to fi bro-fatty replacement impairs RV function and may result in severe pump failure. Gross dilatation of the RV occurs;
- biventricular failure: an advanced stage with involvement of the interventricular septum and LV causing CCF and imitating DCM.
Physical examination
Accurate individual and familiar history, clinical examination, first/second level examinations (12-lead ECG, signal-averaged ECG, 24-hour Holter-ECG, stress test and transthoracic echocardiogram) and third level exams, such as cardiac MR which represents the gold standard for the evaluation.
Diagnosis
The current diagnostic criteria consider 6 categories, which reflect the main characteristics of the disease: structural and functional abnormalities of the RV, depolarization and repolarization abnormalities on the ECG, arrhythmias, histological tissue characterization, family history and genetics. Definite diagnosis is made in presence of 2 major criteria, 1 major and 3 minor or 4 minor criteria.
Diagnostic criteria for arithmogenic cardiomyopathy of the right ventricle new “padua criteria”
| Categories of diagnostic criteria | ACMP (right ventricle) Updated criteria based on ITF modified diagnostic criteria 2010 | ACMP (left ventricle) New Padua Diagnostic Criteria |
| I. Morphological abnormalities of the ventricles | Echo, MRI, or angiography: Major criteria: • RV regional akinesia, dyskinesia, or aneurysm plus one of the following: – global dilatation of the RV (increase in EDV of the RV in accordance with the indexing for age, sex and PPT) according to the data of the imaging study when compared with the nomogram – global contractile dysfunction of the RV (decrease in RV EF in accordance with the nomogram for age and gender) Minor criterion: • Regional akinesia of the pancreas, dyskinesia, or aneurysm of the free wall of the pancreas | Echo, MRI, or angiography: Major criterion: • Global contractile dysfunction (decrease in LVEF according to echocardiography or decrease in global longitudinal deformity of the LV when compared with the nomogram for age, sex and PPT), with or without LV dilatation (increase in LV EDV, indexed to age, sex and PPT) according to imaging research – echocardiography or MRI. Minor criterion: • Regional hypokinesia or akinesia of the free wall of the LV and / or IVS |
| II. Structural myocardial abnormalities | MRI criterion: Major criterion • Transmural contrast delay (fibrosis pattern in one or more pancreatic segments, mandatory confirmation in two orthogonal projections – along the short and long axis). For EMB (limited indications): Major criterion • Fibrous myocardial replacement in one or more samples, with or without fatty infiltration | MRI criterion: Major criterion • Subepicardial or median LV fibrosis (striae pattern, stripes of fibrosis in one or more LV segments according to the “bovine eye” scheme, necessarily in two orthogonal projections) with localization in the septum and / or free LV wall (except for the junction points of the IVS with the ventricles) |
| III. Depolarization anomalies | Major criterion • Inversion of T waves in the right precordial leads (V1, V2, V3) in the absence of complete RBBB (in persons with full pubertal development) Minor criteria • Inversion of T waves in the right precordial leads (V1 and V2) in persons with full pubertal development in the absence of complete RBBB • Inversion of T waves in the right precordial leads (V1, V2, V3 and V4) in persons with full puberty with complete RBBB | Minor criterion • T-wave inversion in the left precordial leads (V4-V6) in the absence of complete LBBB |
| IV. Repolarization anomalies | Major criterion • Inversion of T waves in the right precordial leads (V1, V2, V3) in the absence of complete RBBB (in persons with full pubertal development) precordial leads (V1, V2, V3 and V4) in persons with full pubertal development in the presence of complete RBBB Minor criterion • Inversion of T waves in the left precordial leads (V4-V6) in the absence of complete LBBB | Minor criteria • T-wave inversion in the right precordial leads (V1 and V2) in persons with full pubertal development in the absence of complete RBBB • T-wave inversion in the right precordial leads (V1, V2, V3 and V4) in persons with full pubertal development in the presence of complete RBBB Small criterion • T-wave inversion in the left precordial leads (V4-V6) in the absence of complete RBBB |
| V. Ventricular arrhythmias | Major criterion • Frequent ventricular premature beats (VES> 500 per day), persistent or unstable ventricular tachycardia with LBBB morphology Minor criterion •Frequent ventricular extrasystoles (> 500 per day), unstable or sustained ventricular tachycardia of LBBB morphology with the lower axis (pattern of ectopic substrate of the RV outflow tract) | Minor criterion • Ventricular premature beats (VES> 500 in 24 h), persistent or unstable ventricular tachycardias with RBBB morphology (excluding the “fascicular pattern”) |
| VI. Family history (heredity) / genetics | Major criteria • ACMP was confirmed in first-line relatives with diagnostic criteria • ACMP confirmed histopathologically at autopsy or intraoperatively in a first-line relative • Identification of a pathogenic or possibly pathogenic mutation associated with ACMP in the examined patient Minor criteria • History of ACMP in a first-line family member when it is not possible to determine if the relative’s phenotype meets the diagnostic criteria • Premature sudden death (under the age of 35) with suspected CMP in a first-line relative • ACMP confirmed by histopathological or diagnostic criteria in second-line family members |
Diagnostic Criteria of Arrhythmogenic Right Ventricle Cardiomyopathy (DIAGNOSTIC CRITERIA ITF 2010).
I. Global and regional dysfunction and structural alterations
Major
Echocardiography
- Regional RV akinesia, dyskinesia, or aneurism and 1 of the following (end diastole):
– PLAX RVOT ≥ 32 mm (corrected for body size PLAX/BSA ≥ 19 mm/m2)
– PSAX RVOT ≥ 36 mm (corrected for body size PSAX/BSA ≥ 21 mm/m2)
or RVFAC ≤ 33%
Magnetic Resonance
- Regional RV akinesia or dyskinesia or dyssynchronous RV contraction and 1 of the following:
– Ratio of RV end-diastolic volume to BSA ≥ 110 ml/m2 (male) or ≥ 100 ml/m2 (female) or RV ejection fraction ≤ 40%
RV angiography
- Regional RV akinesia, dyskinesia or aneurysm
Minor
Echocardiography
- Regional RV akinesia or dyskinesia and 1 of the following (end diastole):
PLAX RVOT ≥ 29 to < 32 mm (corrected for body size PLAX/BSA ≥ 16 to < 19 mm/m2)
PSAX RVOT ≥ 32 to < 36 mm (corrected for body size PSAX/BSA ≥ 18 to < 21 mm/m2)
RVFAC >33 to ≤ 40%
Magnetic Resonance
- Regional RV akinesia or dyskinesia or dyssynchronous RV contraction and 1 of the following: Ratio of RV end-diastolic volume to BSA ≥ 100 to < 110 ml/m2 (male) or ≥ 90 to < 100 ml/m2 (female)
or RV ejection fraction >40 to ≤ 45%
II. Tissue characterization
Major
Endomyocardial biopsy
- Residual myocytes < 60% on morphometric analysis (or < 50% if estimated), with fibrous replacement of the RV free wall myocardium in ≥ 1 sample, with or without fatty replacement of tissue
Minor
Endomyocardial biopsy
- Residual myocytes 60% to 75% by morphometric analysis (or 50% to 65% if estimated), with fibrous replacement of the RV free wall myocardium in ≥ 1 sample, with or without fatty replacement of tissue
III. Depolarization abnormalities
Major
Epsilon wave in right precordial leads (V1-V3)
Minor
- Late potentials by SAECG in ≥ 1 of 3 parameters in the absence of a QRS duration of ≥ 110 ms on the standard ECG
- Filtered QRS duration (fQRS) 114 ms
- Duration of terminal QRS < 40 µV (low-amplitude signal duration) ≥ 38 ms
- Root-mean-square voltage of terminal 40 ms ≤ 20 µV
- Terminal activation duration of QRS ≥ 55 ms measured from the nadir of the S wave to the end of the QRS, including R’, in V1, V2, V3 in the absence of complete right bundle-branch block
IV. Repolarization abnomalies
Major
ECG
- Negative Twaves in right precordial leads or beyond in individuals > 14 years of age (in the absence of complete right bundle branch block QRS ≥ 120 ms)
Minor
ECG
- Inverted Twaves in leads V1 and V2 in individuals > 14 years of age (in the absence of complete right bundle-branch block) or in V4, V5, or V6
- Inverted Twaves in leads V1, V2, V3, and V4 in individuals > 14 years of age in the presence of complete right bundle-branch block
V. Ventricular arrhythmias
Major
- Non-sustained or sustained ventricular tachycardia of left bundle-branch morphology with superior axis
Minor
- Non-sustained or sustained ventricular tachycardia of RV outflow configuration, left bundle-branch block morphology with inferior axis or unknown axis
At least 500 ventricular extrasystoles per day at Holter
VI. Family history and genetics
Major
- Definitive diagnosis of ARVC in a first-degree family member (Task Force 2010)
- Autoptic diagnosis (or from transplanted heart analysis) of ARVC in a first-degree family member
- Identification of a pathogenic mutation categorized as associated or probably associated with ARVC in the patient under evaluation
Minor
- History of ARVC in a first-degree relative in whom it is not possible or practical to determine whether the family member meets current Task Force criteria
- Premature sudden death (35 years of age) due to suspected ARVC/D in a first-degree relative
- ARVC confirmed pathologically or by current Task Force Criteria in second-degree relative
* PLAX RVOT = parasternal long-axis right ventricle outflow tract, PSAX = parasternal short-axis, RVFAC = right ventricle fractional area change, RV = right ventricle, SAECG = signal-averaged ECG.
Algorithm for diagnostics of acmp according to new 2020 criteria.
- Right-dominant arrhythmogenic cardiopathy
- Availability of updated APLC criteria (based on modified ITF 2010) – 2 large, 1 large and 2 small, 4 small criteria; the presence of ≥ 1 major or minor criterion from category I or II is required.
- Absence of morphological or structural criteria of LV lesion
- Biventricular ACMP
- Availability of updated criteria for AFA in 2020 based on the modified criteria for ITF 2010 (presence of signs of a definitely accurate or probable diagnosis of AFA)
- The presence of morphological or structural criteria for LV lesion
- Left-dominant arrhythmogenic cardiopathy
- The presence of structural criteria for LV lesion (the presence of a large criterion from category II)
- Verification of pathogenic mutations in ACMP-associated genes
- Absence or minimal involvement of lifespan (according to updated ITF 2010 criteria)
Molecular genetics
- According to the general recommendations for molecular genetic testing in inherited cardiomyopathies, genotyping is indicated to identify a pathogenic or likely pathogenic mutation in a proband who already fulfils phenotypic diagnostic criteria for ARVC, and thus to apply mutation-specific cascade genetic testing for detection of gene carriers among family members.
- Mutation-specific genetic testing is recommended for family members following the identification of a pathogenic or likely pathogenic mutation in the proband with a clinical diagnosis of definite ARVC, to identify genetically affected individuals at a preclinical phase.
Differential diagnosis:
- Idiopathic Ventricular Tachycardia
- Dilated Cardiomyopathy
- Sarcoidosis and myocarditis (ruled out by MR)
- Congenital conditions with right ventricular involvement (Uhl’s disease, Fallot’s Tetralogy)
- Brugada syndrome
- Pulmonary artery hypertension
- Athlete’s heart
- Genetic neuromuscular disorders
Management
There are no established best treatment options for patients with ARVC, and, as the disease is progressive, antiarrhythmic options are used for symptomatic benefit in patients with haemodynamically well-tolerated ventricular arrhythmias.
Excessive training or participation in sport must be avoided.
Antiarrhythmics
B -blockers alone or in combination with class I and III antiarrhythmics. Sotalol and amiodarone have been shown to be most effective.
Radiofrequency ablation
Used to reduce episodes of recurrent monomorphic ventricular tachycardia and ICD shocks in patients who do not respond to medical therapy or if it is contraindicated.
Implantable cardioverter defibrillators
In patients with life-threatening or drug-refractory ventricular arrhythmias and widespread disease, ICDs offer the best protective measure against SCD.
Cardiac Transplantation
In rare, selected, cases there may be a need for heart transplantation due to refractory HF, while incessant ventricular arrhythmias are an infrequent indication.
ICD classification: ICD-11 BC43.6; ICD-10 I42.8
This article is for informational purposes only. Self-medication can be harmful to your health. The use of any drugs mentioned in this article is possible only as directed and under the supervision of a physician.
Register on our website right now to have access to more learning materials!
References:
- Gianfranco Sinagra, Chiara Cappelletto, Antonio DE Luca, Simona Romani, Alessia Paldino, Renata Korcova, Matteo Dal Ferro, Giancarlo Vitrella, Lorenzo Pagnan, Bruno Pinamonti, Focus on arrhythmogenic right ventricular cardiomyopathy, European Heart Journal Supplements, Volume 22, Issue Supplement_L, November 2020, Pages L129–L135, https://doi.org/10.1093/eurheartj/suaa152
- (2012-02). Ramrakha, P., & Hill, J. (Eds.), Oxford Handbook of Cardiology. Oxford, UK: Oxford University Press. Retrieved 22 Aug. 2021, from https://oxfordmedicine.com/view/10.1093/med/9780199643219.001.0001/med-9780199643219.
- Domenico Corrado, Peter J van Tintelen, William J McKenna, Richard N W Hauer, Aris Anastastakis, Angeliki Asimaki, Cristina Basso, Barbara Bauce, Corinna Brunckhorst, Chiara Bucciarelli-Ducci, Firat Duru, Perry Elliott, Robert M Hamilton, Kristina H Haugaa, Cynthia A James, Daniel Judge, Mark S Link, Francis E Marchlinski, Andrea Mazzanti, Luisa Mestroni, Antonis Pantazis, Antonio Pelliccia, Martina Perazzolo Marra, Kalliopi Pilichou, Pyotr G A Platonov, Alexandros Protonotarios, Alessandra Rampazzo, Jeffry E Saffitz, Ardan M Saguner, Christian Schmied, Sanjay Sharma, Hari Tandri, Anneline S J M Te Riele, Gaetano Thiene, Adalena Tsatsopoulou, Wojciech Zareba, Alessandro Zorzi, Thomas Wichter, Frank I Marcus, Hugh Calkins, International Experts, Arrhythmogenic right ventricular cardiomyopathy: evaluation of the current diagnostic criteria and differential diagnosis, European Heart Journal, Volume 41, Issue 14, 7 April 2020, Pages 1414–1429, https://doi.org/10.1093/eurheartj/ehz669
- Ackerman MJ, Priori SG, Willems S, Berul C, Brugada R, Calkins H, Camm AJ, Ellinor PT, Gollob M, Hamilton R, Hershberger RE, Judge DP, Le Marec H, McKenna WJ, Schulze-Bahr E, Semsarian C, Towbin JA, Watkins H, Wilde A, Wolpert C, Zipes DP. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Europace 2011; 13: 1077–1109.
- Corrado D, Perazzolo-Marra M, Zorzi A, et al. Diagnosis of arrhythmogenic cardiomyopathy: The Padua criteria. International Journal of Cardiology. 2020; doi:10.1016/j.ijcard.2020.06.005.
Acute Pulmonary Edema: Emergency Care Algorithm – Should We Remove or Redistribute the Fluid?
Case Presentation: A 64-year-old man was transported to the emergency department by ambulance due to…
Сounseling a patient with suspected Takotsubo-syndrome OSCE guides
The onset of the consultation Wash hands and put on PPE if necessary. Introduce yourself…
Takotsubo syndrome
Takotsubo syndrome is a condition characterized by the sudden onset of acute, transient (lasting up…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…
Symptomatic bradycardia
Symptomatic bradycardia occurs when the heart rate drops below 50 beats per minute. Most often,…
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…