King’s College Criteria for Non- Acetaminophen Toxicity acute hepatic failure
Identification of patients who should be immediately referred for liver transplant.
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
Yes
No
resuscitation (<4 hrs) OR lactate > 3
mmol/L after full fluid resuscitation (12 hours):
Yes
No
96 hours
Yes
No
| Patient’s score | Result | Comment |
|---|---|---|
| 0 | 0 | 0 |
Patients with acute liver failure should be treated in centers that specialize in the care of such patients. The King’s College criteria can help identify patients who require liver transplantation.
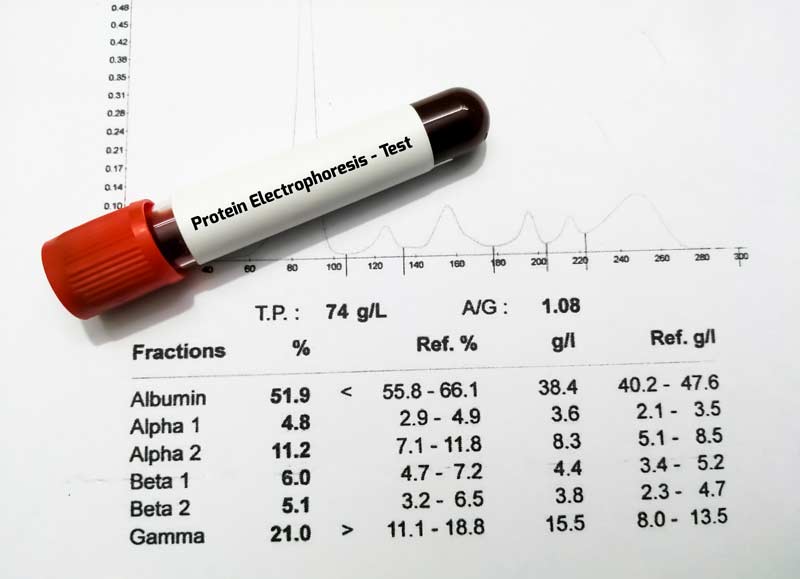
Criteria for non-acetaminophen-induced acute liver failure include:
- 1 big criterion – International normalized ratio (INR)> 6.5; and
- 5 small criteria:
- the patient’s age is <11 or> 40 years;
- the level of bilirubin in serum is more than 300 μmol per liter;
- More than seven days have passed from the onset of jaundice to the development of encelopathy;
- INR (international normalized ratio)> 3.5 (prothrombin time> 50 seconds);
- etiology – the absence of hepatitis A and B or the presence of an idiosyncratic reaction to a drug.
Interpretation of results:
A patient’s survival prognosis is poor if he has at least 1 major criterion or any 3 minor criteria.
The King’s College criteria are recommended by the American Association for the Study of Liver Diseases (AASLD) for determining the need for liver transplantation in patients with acute liver failure.
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
References
- O’Grady JG, Alexander GJ, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989 Aug;97(2):439-45. doi: 10.1016/0016-5085(89)90081-4. PMID: 2490426. https://pubmed.ncbi.nlm.nih.gov/2490426/
- Bernal W, Donaldson N, Wyncoll D, Wendon J. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Lancet. 2002 Feb 16;359(9306):558-63. doi: 10.1016/S0140-6736(02)07743-7. PMID: 11867109. https://pubmed.ncbi.nlm.nih.gov/11867109/
- Bailey B, Amre DK, Gaudreault P. Fulminant hepatic failure secondary to acetaminophen poisoning: a systematic review and meta-analysis of prognostic criteria determining the need for liver transplantation. Crit Care Med. 2003 Jan;31(1):299-305. doi: 10.1097/00003246-200301000-00048. PMID: 12545033. https://pubmed.ncbi.nlm.nih.gov/12545033/
- Schmidt LE, Dalhoff K. Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology. 2002; 36(3):659–665. doi: 10.1053/jhep.2002.35069. https://aasldpubs.onlinelibrary.wiley.com/doi/epdf/10.1053/jhep.2002.35069
- Riordan SM, Williams R. Treatment of hepatic encephalopathy. N Engl J Med. 1997 Aug 14;337(7):473-9. doi: 10.1056/NEJM199708143370707. PMID: 9250851. https://pubmed.ncbi.nlm.nih.gov/9250851/
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
National Institutes of Health Stroke Scale (NIHSS) – Online calculator
The National Institutes of Health Stroke Scale (NIHSS) is a scale designed to assess the…
Charlson Comorbidity Index (CCI) Online Calculator
Charlson Comorbidity Index predicts 10-year survival in patients with multiple comorbidities.
Multiple Myeloma Diagnostic Criteria – Online Calculator
Revised Multiple Myeloma International Staging System (R-ISS) Online Calculator
Revised Multiple Myeloma International Staging System (R-ISS) – prognostication tool for myeloma patients based on…
Multiple Myeloma International Staging System (ISS) Online Calculator
Multiple Myeloma International Staging System (ISS) prognosticates the severity of multiple myeloma based on routinely…