Calgary-Сambridge guide to the medical interview

This manual was developed by specialists from the Faculty of Medicine of the University of Cambridge and the University of Calgary, Canada. It was first published in 1996 (Jonathan Silverman, Suzanne Kurtz).
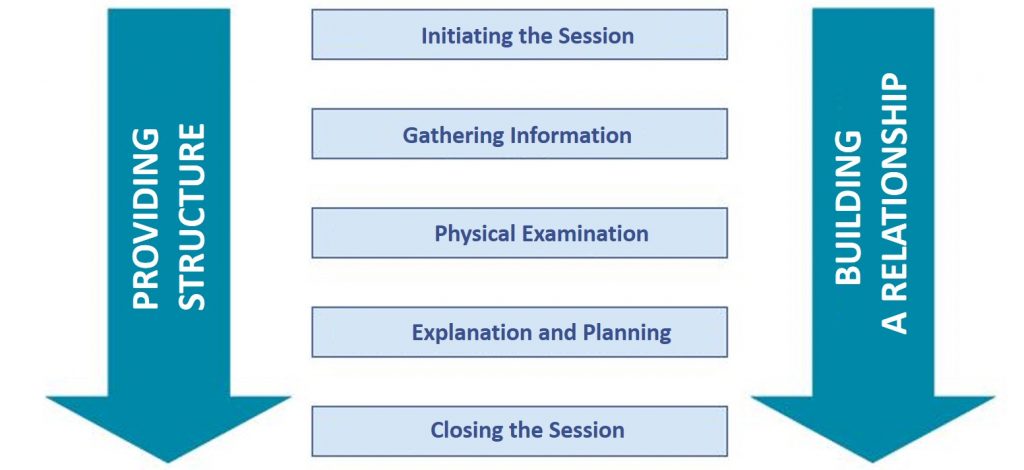
In this consultation model, five stages are distinguished, successively replacing each other (beginning of the consultation, gathering information, review, explanation, and planning, and conclusion of the consultation). At each stage, there are tasks that must be solved using certain skills. There are also two continuous processes that go from the beginning to the end of the consultation (structuring, and building a trusting relationship).
INITIATING THE SESSION
Establishing initial rapport
1. Greets patient and obtains patient’s name
2. Introduces self, role, and nature of interview; obtains consent if necessary
3. Demonstrates respect and interest, attends to patient’s physical comfort
Identifying the reason(s) for the consultation
4. Identifies the patient’s problems or the issues that the patient wishes to address with an appropriate opening question (e.g. “What problems brought you to the hospital?” or “What would you like to discuss today?” or “What questions did you hope to get answered today?”)
5. Listens attentively to the patient’s opening statement, without interrupting or directing the patient’s response
6. Confirms list and screens for further problems (e.g. “so that’s headaches and tiredness; anything else……?”)
7. Negotiates agenda taking both patient’s and physician’s needs into account
GATHERING INFORMATION
Exploration of patient’s problems
8. Encourages patient to tell the story of the problem(s) from when first started
to the present in own words (clarifying the reason for presenting now)
9. Uses open and closed questioning techniques, appropriately moving from open to closed
10. Listens attentively, allowing the patient to complete statements without interruption and leaving space for the patient to think before answering or go on after pausing
11. Facilitates patient’s responses verbally and non–verbally e.g. use of encouragement, silence, repetition, paraphrasing, interpretation
12. Picks up verbal and non–verbal cues (body language, speech, facial expression, affect); checks out and acknowledges as appropriate
13. Clarifies patient’s statements that are unclear or need amplification (e.g. “Could you explain what you mean by light-headed”)
14. Periodically summarises to verify own understanding of what the patient has said; invites the patient to correct interpretation or provide further information.
15. Uses concise, easily understood questions and comments, avoids or adequately explains jargon
16. Establishes dates and sequence of events
Additional skills for understanding the patient’s perspective
17. Actively determines and appropriately explores:
- patient’s ideas (i.e. beliefs re cause)
- patient’s concerns (i.e. worries) regarding each problem
- patient’s expectations (i.e., goals, what help the patient had expected for each problem)
- effects: how each problem affects the patient’s life
18. Encourages patient to express feelings
PROVIDING STRUCTURE
Making organization overt
19. Summarises at the end of a specific line of inquiry to confirm understanding
20. Progresses from one section to another using signposting, and transitional statements; includes the rationale for next section
Attending to flow
21. Structures the interview in a logical sequence
22. Attends to timing and keeping interview on task
BUILDING RELATIONSHIP
Using appropriate non-verbal behavior
23. Demonstrates appropriate non–verbal behavior
- eye contact, facial expression
- posture, position & movement
- vocal cues e.g. rate, volume, tone
24. If reads write notes, or uses a computer, does in a manner that does not interfere with dialogue or rapport
25. Demonstrates appropriate confidence
Developing rapport
26. Accepts legitimacy of patient’s views and feelings; is not judgmental
27. Uses empathy to communicate understanding and appreciation of the patient’s feelings or predicament; overtly acknowledges patient’s views and feelings
28. Provides support: expresses concern, understanding, and willingness to help; acknowledges coping efforts and appropriate self-care; offers partnership
29. Deals sensitively with embarrassing and disturbing topics and physical pain, including when associated with physical examination
Involving the patient
30. Shares thinking with patient to encourage patient’s involvement (e.g. “What I’m thinking now is….”)
31. Explains rationale for questions or parts of physical examination that could appear to be non-sequiturs
32. During physical examination, explains process, asks permission
EXPLANATION AND PLANNING
Providing the correct amount and type of information
33. Chunks and checks: gives information in manageable chunks, checks for understanding, uses patient’s response as a guide to how to proceed
34. Assesses patient’s starting point: asks for patient’s prior knowledge early on when giving information, discovers extent of patient’s wish for information
35. Asks patients what other information would be helpful e.g. aetiology, prognosis
36. Gives explanation at appropriate times: avoids giving advice, information or reassurance prematurely
Aiding accurate recall and understanding
37. Organises explanation: divides into discrete sections, develops a logical sequence
38. Uses explicit categorisation or signposting (e.g. “There are three important things that I would like to discuss. 1st…” “Now, shall we move on to.”)
39. Uses repetition and summarising to reinforce information
40. Uses concise, easily understood language, avoids or explains jargon
41. Uses visual methods of conveying information: diagrams, models, written information and instructions
42. Checks patient’s understanding of information given (or plans made): e.g. by asking patient to restate in own words; clarifies as necessary
Achieving a shared understanding: incorporating the patient’s perspective
43. Relates explanations to patient’s illness framework: to previously elicited ideas, concerns and expectations
44. Provides opportunities and encourages patient to contribute: to ask questions, seek clarification or express doubts; responds appropriately
45. Picks up verbal and non-verbal cues e.g. patient’s need to contribute information or ask questions, information overload, distress
46. Elicits patient’s beliefs, reactions and feelings re information given, terms used; acknowledges and addresses where necessary
Planning: shared decision making
47. Shares own thinking as appropriate: ideas, thought processes, dilemmas
48. Involves patient by making suggestions rather than directives
49. Encourages patient to contribute their thoughts: ideas, suggestions and preferences
50. Negotiates a mutually acceptable plan
51. Offers choices: encourages patient to make choices and decisions to the level that they wish 52. Checks with patient if accepts plans, if concerns have been addressed
CLOSING THE SESSION
Forward planning
53. Contracts with patient re next steps for patient and physician
54. Safety nets, explaining possible unexpected outcomes, what to do if plan is not working, when and how to seek help
Ensuring appropriate point of closure
55. Summarises session briefly and clarifies plan of care
56. Final check that patient agrees and is comfortable with plan and asks if any corrections, questions or other items to discuss
OPTIONS IN EXPLANATION AND PLANNING (includes content)
Discussing investigations and procedures
57. Provides clear information on procedures, eg, what patient might experience, how patient will be informed of results
58. Relates procedures to treatment plan: value, purpose
59. Encourages questions about and discussion of potential anxieties or negative outcomes
Discussing opinion and significance of problem
60. Offers opinion of what is going on and names if possible
61. Reveals rationale for opinion
62. Explains causation, seriousness, expected outcome, short and long-term consequences
63. Elicits patient’s beliefs, reactions, concerns re opinion
Negotiating mutual plan of action
64. Discusses options eg, no action, investigation, medication or surgery, non-drug treatments (physiotherapy, walking aides, fluids, counselling, preventive measures)
65. Provides information on action or treatment offered. Name steps involved, how it works benefits and advantages possible side effects
66. Obtains patient’s view of need for action, perceived benefits, barriers, motivation
67. Accepts patient’s views, advocates alternative viewpoint as necessary
68. Elicits patient’s reactions and concerns about plans and treatments including acceptability
69. Takes patient’s lifestyle, beliefs, cultural background and abilities into consideration
70. Encourages patient to be involved in implementing plans, to take responsibility and be self-reliant
71. Asks about patient support systems, discusses other support available
References:
- Kurtz SM, Silverman JD, Draper J (1998) Teaching and Learning Communication Skills in Medicine. Radcliffe Medical Press (Oxford)
- Silverman JD, Kurtz SM, Draper J (1998) Skills for Communicating with Patients. Radcliffe Medical Press (Oxford)
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
ClinCaseQuest Featured in SchoolAndCollegeListings Directory
Exciting News Alert! We are thrilled to announce that ClinCaseQuest has been successfully added to…
We presented our experience at AMEE 2023
AMEE 2023 took place from 26-30 August 2023 at the Scottish Event Campus (SEC), Glasgow,…
We are on HealthySimulation – world’s premier Healthcare Simulation resource website
We are thrilled to announce that our Simulation Training Platform “ClinCaseQuest” has been featured on…
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
National Institutes of Health Stroke Scale (NIHSS) – Online calculator
The National Institutes of Health Stroke Scale (NIHSS) is a scale designed to assess the…
SESAM 2023 Annual Conference
We are at SESAM 2023 with oral presentation “Stage Debriefing in Simulation Training in Medical…