Infective endocarditis. Diagnostic criteria for infective endocarditis

Infective endocarditis (IE) is defined as an infection of the endocardial surfaces of the heart—primarily of 1 or more heart valves, the mural endocardium, or a septal defect. Its intracardiac effects include severe valvular insufficiency, intractable congestive heart failure, and myocardial abscesses. If left untreated, IE is inevitably fatal.
Risk factors for infective endocarditis |
|
High risk |
Prosthetic valves Previous bacterial endocarditis Aortic valve disease Mitral regurgitation or mixed mitral disease Cyanotic congenital heart disease Patient ductus arteriosis Uncorrected left → right shunt Intracardiac or systemic pulmonary shunts |
Moderate risk |
Mitral valve prolapse with regurgitation or valve thickening Isolated mitral stenosis Tricuspid valve disease Pulmonary stenosis Hypertrophic cardiomyopathy
Degenerative valve disease in elderly Mitral thrombus (e.g. post infarction) |
Low risk |
Mitral valve prolapse without regurgitation Tricuspid incompetence without structural abnormality Isolated atrial septal defect Surgically corrected left → right shunt with no residual shunt Calcification of mitral valve annulus Ischemic heart disease and/or previous coronary artery bypass graft (CABG) Permanent pacemaker Atrial myxoma |
Other predisposing factors: · Arterial prosthesis or arteriovenous fistulae · Recurrent bacteremia (e. g. IV drug users, severe periodontal disease, colon carcinoma) · Conditions predisposing to infections (e.g. diabetes, renal failure, alcoholism, immunosuppression) · Recent central line In many cases no obvious risk factor is identified! |
|
Diagnosis of endocarditis
Key facts!
- Clinical features can be non-specific and diagnosis difficult.
- Maintain a high index of suspicion in patients presenting with unexplained fever, a predisposing cardiac lesion, bacteremia, and embolic phenomena.
Duke classification
- Developed in 1994 and modified in 2000 as a means of standardizing the diagnosis of IE.
- This classification has a sensitivity of approximately 80% overall when the criteria are evaluated at the end of patient follow-up in epidemiological studies.
- However, the modified Duke criteria show a lower diagnostic accuracy for early diagnosis in clinical practice, especially in the case of prosthetic valve endocarditis (PVE) and pacemaker or defibrillator lead IE.
- Cardiac/whole-body computer tomography (CT) scan, cerebral MRI, 18F-FDG PET/CT, and radiolabeled leukocyte SPECT/CT might improve the detection of silent vascular phenomena as well as endocardial lesions.
- The addition of the results of these imaging modalities may improve the sensitivity of the modified Duke criteria in difficult cases.
Definitions of the terms used in the European Society of Cardiology 2015 modified criteria for the diagnosis of infective endocarditis
| Major criteria |
| I. Blood cultures positive for IE a. Typical microorganisms consistent with IE from 2 separate blood cultures: • Viridans streptococci, Streptococcus gallolyticus (Streptococcus bovis), Staphylococcus aureus; or • Community-acquired enterococci, in the absence of a primary focus; or b. Microorganisms consistent with IE from persistently positive blood cultures: • ≥2 positive blood cultures of blood samples drawn >12 h apart; or • All of 3 or a majority of ≥4 separate cultures of blood (with and last samples drawn ≥1 h apart); or • Single positive blood culture for Coxiella burnetii or phase I IgG antibody titer >1:800. |
| II. Imaging positive for IE a. Echocardiogram positive for IE: • Vegetation • Abscess, pseudoaneurysm, intracardiac • Valvular perforation or aneurysm • New partial dehiscence of prosthetic valve. b. Abnormal activity around the site of prosthetic valve implantation detected by 18F-FDG PET/CT (only if the prosthesis was implanted for >3 months) or radiolabeled leukocytes SPECT/CT. c. Define paravalvular lesions by cardiac CT. |
| Minor criteria |
| 1. Predisposition such as predisposing heart condition, or injection drug use. 2. Fever as temperature >38°C. 3. Vascular phenomena (including those detected by imaging only): major arterial emboli, septic pulmonary infarcts, infectious (mycotic) aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway’s lesions. 4. Immunological phenomena: glomerulonephritis, Osler’s nodes, Roth’s spots, and rheumatoid factor. 5. Microbiological evidence: positive blood culture but does not meet a major criterion as noted above or serological evidence of active infection with organism consistent with IE. |
Definition of infective endocarditis according to the modified Duke criteria (adapted from Li et al.)
| Definite IE |
| Pathological criteria: • Microorganisms demonstrated by culture or on histological examination of a vegetation, a vegetation that has embolized, or an intracardiac abscess specimen; or • Pathological lesions; vegetation or intracardiac abscess by histological examination showing active endocarditis| Clinical criteria: • 2 major criteria; or • 1 major criterion and 3 minor criteria; or • 5 minor criteria |
| Possible IE |
| • 1 major criterion and 1 minor criterion; or • 3 minor criteria |
| Rejected IE |
| • Firm alternate diagnosis; or| • Resolution of symptoms suggesting IE with antibiotic therapy for ≤4 days; or • No pathological evidence of IE at surgery or autopsy, with antibiotic therapy for ≤4 days; or • Does not meet criteria for possible IE, as above |
| *The identification of paravalvular lesions by cardiac CT should be considered a major criterion. *In the setting of the suspicion of endocarditis on a prosthetic valve, abnormal activity around the site of implantation detected by 18F-FDG PET/CT (only if the prosthesis was implanted for 3 months) or radiolabeled leucocyte SPECT/ CT should be considered a major criterion. *The identification of recent embolic events or infectious aneurysms by imaging only (silent events) should be considered a minor criterion. |
Investigation of endocarditis
| Blood cultures | Take 3-4 sets of culture from different sites at least an hour apart and inoculate a minimum of 10mL/bottle for the optimal pick-up rate. Both aerobic and anaerobic bottles must be used. Lab should be advised that IE is a possibility, especially if unusual organism is suspected. In stable patients on antibiotic therapy, doses must be delayed allowing culture on successive days. Ask for prolonged (fungal) culture in IV drugs users. When a microorganism has been identified, blood cultures should be repeated after 48–72 h to check the effectiveness of treatment. |
| Full blood count | May show normochromic, normocytic anemia (exclude hematinic deficiency), neutrophil leukocytosis, and perhaps thrombocytopenia. |
| Urea and electrolytes | May be deranged (this should be monitored throughout treatment). |
| Liver function tests | May be deranged, especially with an increase in alkaline phosphatase (ALP) and gamma glutamyl transferase (GGT). |
| Erythrocyte sedimentation rate /C-reactive protein/ procalcitonin | Acute phase reaction and sepsis indicator |
| Urinalysis | Microscopic hematuria ± proteinuria |
| Immunology | Polyclonal elevation in serum Igs, complement levels |
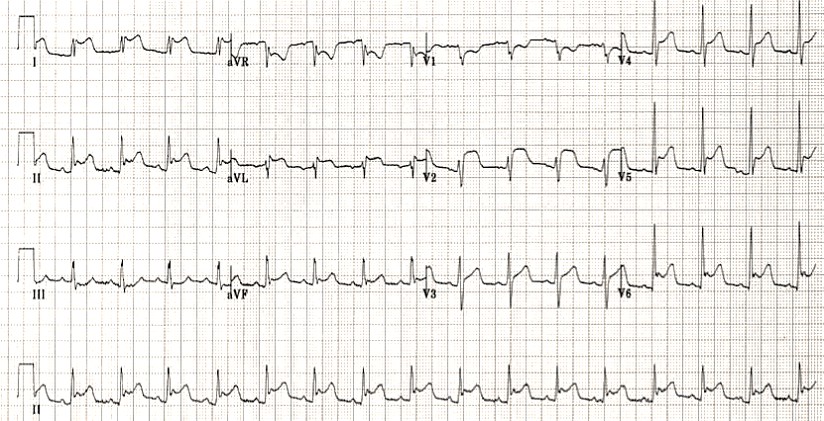
| Electrocardiogram | May have changes associated with any underlying cause. There may be atrioventricular block or conduction defects (especially aortic root absence) and, rarely (embolic), acute myocardial infarction. |
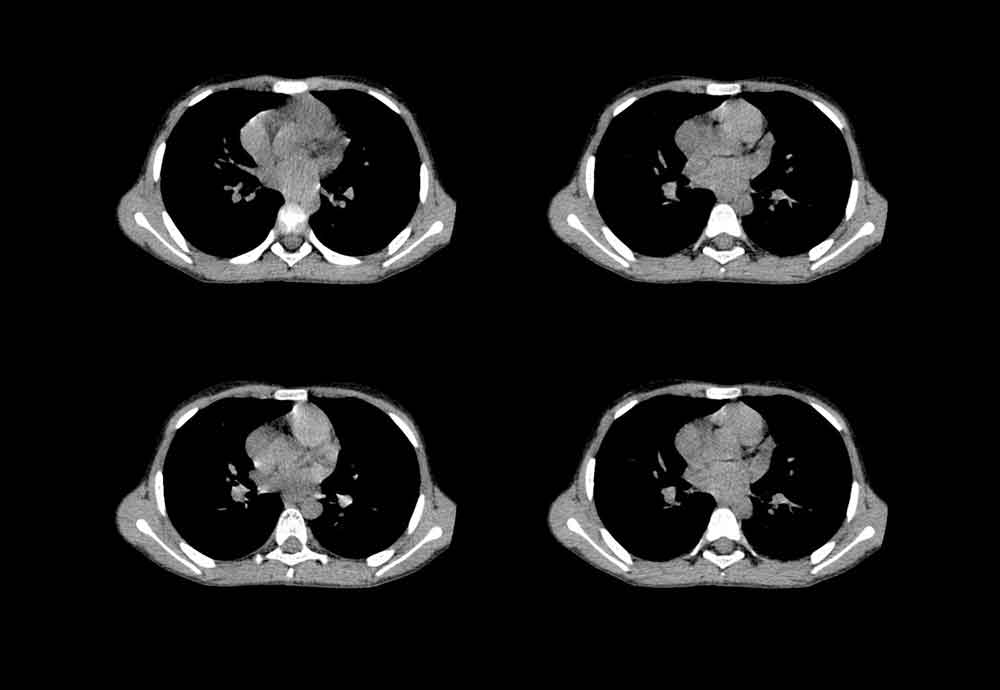
| Chest X-ray | May be normal. Look for pulmonary oedema or multiple infected or infarcted areas from septic emboli (tricuspid endocarditis). |
| Echocardiography (ECHO) | Transthoracic ECHO may confirm the presence of valve lesions and/or demonstrate vegetations if .2 mm in size. Transesophageal echocardiography is more sensitive for aortic root abscess and mitral leaflet involvement. A normal ECHO does not exclude the diagnosis. If the suspicion for IE remains high despite negative TEE findings, a repeat TEE should be performed after 3 to 5 days. Furthermore, repeat TEE should be performed if a new intracardiac complication is suggested by clinical features. Performance of TTE is also reasonable upon completion of antibiotic therapy for the establishment of a new baseline. Three echocardiographic findings are major criteria in the diagnosis of IE: vegetation, abscess or pseudoaneurysm and new dehiscence of a prosthetic valve. |
| Magnetic resonance imaging | Useful in investigation of paravalvular extension, aortic root aneurysm and fistulas. Systematic cerebral MRI has an impact on the diagnosis of IE since it adds one minor Duke criterion. |
| Nuclear imaging | With the introduction of hybrid equipment for both conventional nuclear medicine [e.g. single-photon emission CT (SPECT)/CT] and PET (i.e. PET/CT), nuclear molecular techniques are evolving as an important supplementary method for patients with suspected IE and diagnostic difficulties. Radiolabeled WBC SPECT/CT is more specific for the detection of IE and infectious foci than 18F-FDG PET/CT and should be preferred in all situations that require enhanced specificity. |
| Dentition | All patients should have an orthopantomogram – a panoramic dental X-ray and a dental opinion. |
| Swabs | Any potential sites of infection (skin lesion). |
| Ventilation/perfusion (V/Q) scan | In cases when right-sided endocarditis is suspected, this may show multiple mismatched defects. |
| Histological diagnosis of infective endocarditis | Pathological examination of resected valvular tissue or embolic fragments remains the gold standard for the diagnosis of IE. |
| Save serum for | Aspergillus precipitins; Candida antibodies (rise in titer); Q fever (Coxiella burnetti) compliment fixation test; Chlamydia complement fixation test; Brucella agglutinins; Legionella antibodies; Bartonella species. |
Literature:
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. American Journal of Medicine. 96(3):200-9, 1994.
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000 Apr;30(4):633-8. doi: 10.1086/313753. Epub 2000 Apr 3. PMID: 10770721.
- Yehuda Adler, Philippe Charron, Massimo Imazio, Luigi Badano, Gonzalo Barón-Esquivias, Jan Bogaert, Antonio Brucato, Pascal Gueret, Karin Klingel, Christos Lionis, Bernhard Maisch, Bongani Mayosi, Alain Pavie, Arsen D Ristić, Manel Sabaté Tenas, Petar Seferovic, Karl Swedberg, Witold Tomkowski, ESC Scientific Document Group, 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS), European Heart Journal, Volume 36, Issue 42, 7 November 2015, Pages 2921–2964, https://doi.org/10.1093/eurheartj/ehv318
- Thornhill MH, Gibson TB, Cutler E, Dayer MJ, Chu VH, Lockhart PB, et al. Antibiotic Prophylaxis and Incidence of Endocarditis Before and After the 2007 AHA Recommendations. J Am Coll Cardiol. 2018 Nov 13. 72 (20):2443-2454. [Medline].
- https://emedicine.medscape.com/article/216650-guidelines
Register on our website right now to have access to more learning materials!
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
SAVED VTE Score
SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…
IMPEDE VTE Score
IMPEDE score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…
Chest CT Scan
To analyze a CT scan of the chest, imagine that the patient is lying on…
X-ray Heart Borders
According to the radiograph of the chest, the boundaries of the heart are formed: The…
Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents /OSCE guide
Opening the consultationWash your hands and don PPE if appropriateIntroduce yourself to the patient including…