Сounseling a patient with suspected Takotsubo-syndrome OSCE guides

The onset of the consultation
- Wash hands and put on PPE if necessary.
- Introduce yourself to the patient by stating your name and role.
- Confirm the patient’s last name, first name, and date of birth.
- Explain what the examination will involve using language the patient can understand.
- Get consent for consultation.
- Adequately expose the patient for examination.
- Ask the patient if he is in pain before proceeding with the clinical examination.
Clarification of the main complaint
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
- Analyze the patient’s thoughts, fears, and expectations
- Summarize the patient’s complaints
Comprehensive assessment
- Assess other symptoms to get a comprehensive picture
Medical history
- Find out when and how the chest pain first appeared; what, according to the patient, could have caused its appearance (pay special attention to psychological or physical stress); specify whether the patient sought medical help, if so, to whom and what was the end of his appeal, if not, then specify why the patient did not seek medical help; whether he took medical drugs on his own or as prescribed by a doctor, if so, whether the nature of complaints changed against the background of treatment
- In the case of hospitalization for chest pain, read the extract from the patient’s medical history, pay attention to the established clinical diagnosis, the results of laboratory or instrumental examinations, the treatment and recommendations after discharge
- If the patient has previously undergone laboratory or instrumental examinations for current complaints, analyze their results and indicate important findings
- Find out what prompted the patient to contact you
- Exclude other causes of chest pain by asking the patient clarifying questions
History of life
- The accuracy of the presence of previously diagnosed cardiovascular diseases in the patient, in particular myocardial infarction, stroke, rhythm disorders, cardiomyopathy, angina pectoris, arterial hypertension
- Find out whether the patient suffers from mental health disorders, such as depression, anxiety, or schizophrenia, which are risk factors for the development of Takotsubo syndrome
- Determine whether the patient has chronic diseases, in particular diabetes, bronchial asthma, and chronic obstructive pulmonary disease, which are risk factors for the development of Takotsubo syndrome
- Determine whether the patient is taking medications that stimulate the sympathetic nervous system (eg, beta 2-adrenergic receptor agonists, alpha 1-adrenergic receptor agonists, serotonin and norepinephrine reuptake inhibitors, epinephrine)
- Determine whether the patient is abusing psychotropic substances (eg, cannabis, cannabinoids)
- Find out whether the menstrual function is preserved; if not, find out the time of menopause and whether the patient is taking hormone replacement therapy
- Check whether the patient has undergone surgery
- Find out if the patient had any injuries, find out how the recovery period went
- Find out whether the patient has a drug intolerance and specify how it manifests itself
- Find out whether the patient has bad habits – drinking alcohol, narcotic substances, smoking
- Find out the family status of the patient, living conditions, and psychological problems in the family; find out if there were any blood relatives of the patient with cardiovascular diseases
- Find out whether the patient works, his profession, conditions, and nature of work, and whether the work is related to physical or psychological overload
Objective examination:
- Assessment of the patient’s general condition (satisfactory, moderate, severe, very severe).
- General examination of the patient:
- Consciousness, the position of the patient, gait, and posture.
- Physique, type of constitution, height, weight, body mass index.
- Skin and visible mucous membranes (color, rash, scars, scratches), elasticity and moisture of the skin, condition of skin derivatives, and development of subcutaneous adipose tissue.
- Pastiness, edema.
- Lymph nodes.
- Muscular system: development of muscles, their tone, presence of atrophy, soreness.
- Joints: examination, palpation, measurement of limbs and joints, determination of the degree of joint mobility.
- Examination of the head, face, and neck with an assessment of the state of the thyroid gland.
- Research of organ systems
- Research of respiratory organs
- Research of circulatory organs.
- Research of digestive organs.
- Examination of the urinary system
- Assessment of the probability of Takotsubo syndrome
Laboratory tests
- Clinical blood count with leukocyte formula and calculation of ESR (erythrocyte sedimentation rate)
- Biochemical blood analysis (total protein, creatinine, urea, alanine aminotransferase, aspartate aminotransferase, glucose, alkaline phosphatase, uric acid, bilirubin with fractions)
- Blood electrolytes (K+ and Na+)
- Lipid profile
- Coagulogram
- Blood test for troponin I / T
- Blood test for creatine phosphokinase (CK)
- Blood analysis for brain natriuretic peptide ( BNP ) or the N-terminal precursor of brain natriuretic peptide ( NT – pro-BNP )
- Assessment of thyroid gland function (thyroid-stimulating hormone-TSH) (according to indications)
- Urine analysis with sediment microscopy (as indicated)
- Pregnancy test for patients of childbearing age (according to indications)
Instrumental diagnostic tests
- Electrocardiography
- Transthoracic echocardiography
- Coronarography
- Ventriculography
- MRI of the heart
- CT angiography of coronary arteries
Making a clinical diagnosis
- Carrying out differential diagnosis
- Assessment of diagnostic criteria
- Determination of the anatomical variant
- Definition of complications
- Making of clinical diagnosis
Specialist consultations
- Cardiologist
- Interventional cardiologist
- Radiologist
- Psychotherapist
- Psychiatrist
- Endocrinologist
- Narcologist
- Gynecologist
- Doctor of physical and rehabilitation medicine
Purpose of treatment
- Supportive therapy
- Treatment of complications
- Prevention of relapse
Consulting and support
- Informing the patient about the disease
- Discussion of research results with the patient
- Explanation to the patient of the possible cause of the disease
- Explanation to the patient of possible symptoms that may occur during the disease
- Explanation to the patient of the possible consequences of the disease
- Explaining the available treatment methods, informing the patient about the risks and benefits of different treatment methods
- Answers to the patient’s questions
- Explanation of the scope of monitoring during and after treatment
- Appointment of regular checks and controls to assess the effectiveness of treatment and changes in the patient’s condition
End of consultation
- Summarize the data and ask the patient if anything important has been missed
- Inform the patient about further tactics
- Thank the patient
- Dispose of PPE properly and wash hands
Key communication skills
- Active listening
- Summing up
- Selection of indicative signs
Join our Simulation Training to gain clinical experience
Clinical case simulator “An interrupted symphony”
Medical training. A 74-year-old patient was brought to the hospital by the medical team, presenting…
Clinical case simulator “Mysteries of the heart”
Medical training. A 51-year-old female patient was brought by an emergency medical team to a…
From diagnosis to remission
A 34-year-old male patient was admitted to a hospital department presenting with symptoms of general…
A case of treatment of a patient with blood test abnormalities and fever
A 52-year-old man was admitted to the hematological center with a suspicion of a hematological…
A patient with severe neurological symptoms in the hematology department
A 69-year-old woman was hospitalized to the hematology department of the hospital with complaints of…
Choosing a treatment strategy for a patient with abnormalities in complete blood count
A 46-year-old woman was referred to a hematologist by her family doctor. The patient complains…
From chest pain to diagnosis in a 61-year-old patient
A 61-year-old woman consulted a hematologist with complaints of chest pain, weight loss, and general…
Objective structured clinical examination (OSCE)
Objective Structured Clinical Examination (OSCE) is a modern type of knowledge assessment used in medicine….
Cardiac pain and ECG changes. What can be detected from an ECG?
A 53-year-old man with a past medical history of diabetes and hypertension presents to the…
Unconsciousness and ECG changes in a patient with comorbidities
The patient was admitted to the cardiology department, where he received an appropriate treatment. After…
Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in a young woman
Case simulator Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in…
Pregnancy after myocardial revascularization
Clinical case simulator “Pregnancy after myocardial revascularization”. A young woman who has had multiple recurrent…
Chronic Myeloid Leukemia and Jaundice
A patient diagnosed with chronic myeloid leukemia suddenly develops jaundice. Is this a manifestation of…
Back pain in a woman
Simulator of a clinical case “Back pain in a woman”: the patient cries, having learned…
A Lady with a sudden cardiac pain
A sudden cardiac pain: what could have happened to Miss Laura Smith? What are the…
The rehabilitation program in patients with acute myocardial infarction
This scenario is a simulation of the clinical situation “The rehabilitation program in patients with…
Assessment the degree of ST segment elevation on the ECG, J-point
Do you know how to assess the degree of ST segment elevation on an ECG?…
The onset of the consultation
- Wash hands and put on PPE if necessary.
- Introduce yourself to the patient by stating your name and role.
- Confirm the patient’s last name, first name, and date of birth.
- Explain what the examination will involve using language the patient can understand.
- Get consent for consultation.
- Adequately expose the patient for examination.
- Ask the patient if he is in pain before proceeding with the clinical examination.
Examination for Takotsubo syndrome is conducted when characteristic clinical symptoms and objective signs of this condition are present.
Typical clinical symptoms of Takotsubo syndrome include:
- Symptoms of myocardial ischemia (chest pain)
- Symptoms of heart failure (shortness of breath, sensation of air hunger)
- Symptoms of cerebral hypoperfusion (dizziness, loss of consciousness)
Clarification of the main complaint
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
- Analyze the patient’s thoughts, fears, and expectations
- Summarize the patient’s complaints
- Use open-ended questions to explore the patient’s complaints
- Details of the main complaint
The most common complaint of a patient with Takotsubo syndrome is chest pain. To detail this complaint, follow this algorithm:
- Localization: find out where it hurts
- Onset: find out how the pain started – suddenly or gradually
- Nature: Ask the patient to describe how he/she feels the pain.
- Irradiation: Find out if the pain is spreading
- Accompanying symptoms: find out if there are other symptoms that accompany the pain
- Dynamics over time: Determine whether the pain has changed over time
- Factors that make the pain worse or worse: Find out if there is anything that makes the pain worse or worse
“Can you show me precisely where it hurts?”
“Could you describe this pain?”
Is this pain constant or intermittent?
“How long does the pain typically last?“
“Does the pain radiate to other areas?“
“What typically triggers the onset of this pain?“
“What measures provide relief from this pain?“
“Are there any other symptoms accompanying the pain?”
To detail the complaint of chest pain, we recommend using the SOCRATES questionnaire. An example survey is given below.
| S | Site (Localization) | Ask about the location of the pain | “Where does it hurt?” “Can you tell me precisely where you feel the pain?” “Can you show me where it hurts?” “Where is the pain localized?” |
| O | Onset | Specify how and when the pain occurred | “Did the pain come on suddenly or develop gradually?” “When did the pain first occur?” “When did the symptoms first appear?” “Did the pain occur at rest or during physical activity?” “How long did the pain last?” “How and when did it start?” “Did the pain start suddenly, or did it develop gradually?” “What were you doing precisely when the pain began?” “What triggers the onset of pain for you?” “When does the pain typically occur?” “Under what circumstances does the pain worsen?” |
| C | Character | Ask about specific characteristics of the pain | “How would you describe this pain?” “Is the pain continuous or does it come and go?” “Could you describe the pain to me?” “Can you describe the nature of the pain?” |
| R | Radiation (Irradiation) | Ask if the pain is radiating | “Does the pain radiate elsewhere?” “Does it spread or radiate?” “Where exactly does the pain spread?” “To which part of the body does the pain radiate?” |
| A | Associated symptoms | Ask if there are any symptoms related to pain | “Are there any other symptoms associated with the pain?” “Do you experience any other symptoms besides pain?” “What other symptoms are you experiencing?” “Are there any other symptoms apart from the pain?” |
| T | Time course ( dynamics over time ) | Find out how the pain has changed over time | “Has the pain changed over time?” |
| E | Exacerbating or relieving factors | Ask if there is anything that makes the pain worse or worse | “Does anything exacerbate the pain?” “Does anything alleviate the pain?” |
| S | Severity | Determine the intensity of the pain by asking the patient to rate it on a scale of 0 to 10 | “How would you rate the pain on a scale of 0 to 10, where 0 is no pain and 10 is the worst pain you have ever felt?” “Please rate the intensity of the pain on a scale from 0 to 10, where 0 means no pain and 10 represents the most severe pain you have ever experienced.” “On a scale of 1 to 10, how severe is the pain?” “Could you rate the intensity of the pain on a scale from 1 to 10?” |
Some elements of the SOCRATES acronym can be used to detail a complaint of shortness of breath.
| S | Site (Localization) | – | – |
| O | Onset | Specify how and when the shortness of breath occurred | “Did the shortness of breath come on suddenly or gradually?” “When did you first experience shortness of breath?” “What do you think caused the shortness of breath to start?” |
| C | Character | Assess the nature of shortness of breath | “How would you describe your experience of shortness of breath?” “Can you describe in detail how you feel when you experience shortness of breath?” “Could you describe specifically what sensations you feel?” |
| R | Radiation (Irradiation) | – | – |
| A | Associated symptoms | Ask if there are other symptoms associated with shortness of breath | “Do you experience any other symptoms alongside the shortness of breath?” “Have you noticed any coughing along with the shortness of breath?” “Do you feel any chest pain when experiencing shortness of breath?” “Have you noticed any blood in your sputum when experiencing shortness of breath?” |
| T | Time course ( dynamics over time ) | Find out if the shortness of breath has changed over time | “Has the shortness of breath changed over time?” |
| E | Exacerbating or relieving factors | Ask if there is anything that makes the shortness of breath worse or worse | “What can cause an increase in shortness of breath?” “What exacerbates shortness of breath?” “What relieves shortness of breath?” “Under what conditions does shortness of breath increase?” “Does shortness of breath worsen when lying down?” “Does shortness of breath increase during physical exertion?” “Does changing body position affect the severity of shortness of breath?” |
| S | Severity | Determine the intensity of dyspnea by asking the patient to rate it on a scale of 0 to 10 | “Estimate the severity of shortness of breath on a scale from 0 to 10, where 0 is the absence of shortness of breath, and 10 is the strongest shortness of breath at rest.” “Can you describe the intensity of shortness of breath on a scale of 1 to 10?” |
Analyze the patient’s thoughts, fears, and expectations
A key component of history taking involves exploring the patient’s thoughts, concerns, and expectations to gain insight into how they currently perceive their condition, their worries, and what they anticipate from the consultation.
The exploration of thoughts, concerns, and expectations should be flexible throughout the consultation, responding to cues from the patient. This approach ensures that your consultation remains patient-oriented rather than formulaic.
It’s important to structure the analysis of thoughts, fears, and expectations in a way that feels natural during your consultation.
| Reflections | Explore the patient’s perception of the current problem | “What do you think could have caused these symptoms?” “Do you have any guesses as to the cause of these symptoms?” |
| Concern | Explore the patient’s current concerns | • “Is there something that bothers you?” • “How do you cope with everyday activities?” “Is there anything you and I haven’t discussed yet?” |
| Expectation | Ask what the patient hopes to gain from the consultation | • “How can I help you today?” • “What do you expect from today’s consultation?” • “What do you think would be the best course of action?” |
Summarize the patient’s complaints
Summarize what the patient told you about his complaint. This allows you to check how correctly you understood the patient’s complaints and gives the patient the opportunity to correct any inaccurate information.
When you have concluded, ask the patient if there is anything else you missed. Periodically, as the consultation progresses, summarize intermediate results.
Comprehensive assessment
- Screen for symptoms of damage to other organs and systems
A comprehensive assessment includes a brief survey of the patient for symptoms of other systems that may or may not be related to the chief complaint. This comprehensive examination also helps identify symptoms that the patient may have forgotten to mention.
Deciding which symptoms to inquire about depends on the presenting complaint and your level of experience.
Here are some examples of symptoms that you might inquire about for each system:
| System | Symptoms |
| General manifestations | fever, weight change, fatigue, sweating, general weakness |
| Respiratory | shortness of breath, cough, sputum, wheezing, hemoptysis, pleuritic chest pain |
| Cardiovascular | chest pain, shortness of breath, heart failure, palpitations, swelling of the lower extremities |
| Gastrointestinal | dyspepsia, nausea, vomiting, dysphagia, abdominal pain, stool disorders |
| Genitourinary | oliguria, polyuria, nocturia, pain during urination |
| Neurological | changes in vision, motor or sensory disturbances, headache |
| Locomotor | pain in the chest wall, bone pain, trauma |
| Skin | rashes, ulcers, hemorrhages, petechiae, bruises, hemorrhages, neoplasms |
Medical history
- Find out when and how the chest pain first appeared; what, according to the patient, can cause its appearance (pay special attention to psychological or physical stress experienced); specify whether the patient sought medical help, if so, to whom and what was the end of his application, if not, then specify why he did not seek help; whether he took medical drugs on his own or as prescribed by a doctor, if so, whether the nature of the complaints changed against the background of treatment
“When did the chest pain start for you?”
“What do you think might have caused it to start?”
“Did you seek medical assistance?”
- In the case of hospitalization for chest pain, read the extract from the patient’s medical history, pay attention to the established clinical diagnosis, the results of laboratory or instrumental examinations, the treatment and recommendations after discharge
- If the patient has previously undergone laboratory or instrumental examinations for current complaints, analyze their results and indicate important findings
- Find out what prompted the patient to contact you
“What made you decide to reach out to me?”
- Exclude other causes of existing symptoms by asking the patient clarifying questions
“Did you have a fever?”
“Is the chest pain accompanied by nausea or the urge to vomit?”
Other causes of chest pain:
- Acute coronary syndrome (ACS)
Acute coronary syndrome is characterized by complaints of intense chest pain radiating to the left arm, left shoulder, left scapula, neck, and epigastrium, lasting more than 20 minutes, not relieved by taking nitrates, and often accompanied by shortness of breath, a feeling of fear, and increased sweating. The pain syndrome in ACS is very similar to the pain syndrome in Takotsubo syndrome, which creates significant difficulties for differential diagnosis.
- Acute myocarditis
Clinical symptoms such as chest pain, shortness of breath, and palpitations are characteristic of both Takotsubo syndrome and myocarditis. The pain syndrome in myocarditis is very similar to the pain syndrome in Takotsubo syndrome, which makes it challenging to differentiate these two conditions based solely on this criterion. However, it should be noted that myocarditis is characterized by the presence of a recently acquired infectious disease, which is not typically associated with Takotsubo syndrome. Conversely, in Takotsubo syndrome, the onset of pain is often preceded by psychological or physical stress.
- Angina
Angina is characterized by chest pain radiating to the left arm, left shoulder, left shoulder blade, neck, and epigastrium. However, in angina, the pain typically lasts up to 20 minutes and subsides with rest or after taking nitrates. In contrast, in Takotsubo syndrome, the pain persists for a longer duration and is not relieved by nitrates.
- Thromboembolism of the pulmonary artery
For thromboembolism of the pulmonary artery and Takotsubo syndrome, chest pain often accompanied by shortness of breath and a sensation of breathlessness is characteristic. The nature of the pain in both conditions is anginal, posing a challenge for differential diagnosis. Considering that the primary cause of pulmonary embolism (PE) is typically deep vein thrombosis in the lower extremities, it’s essential to consider typical symptoms such as unilateral pain and swelling of the affected lower limb, along with an increase in its size.
- Dissecting aneurysm of the aorta
Patients with a dissecting aortic aneurysm typically present with sudden, excruciating, tearing chest pain that radiates to the neck, back, and lower limbs, often in a migratory pattern. While the pain in Takotsubo syndrome can also be intense, it is typically not as severe as in a dissecting aortic aneurysm.
- Acute pericarditis
The clinical presentation of acute pericarditis shares many similarities with that of Takotsubo syndrome, as both conditions typically involve chest pain and shortness of breath. However, acute pericarditis is distinguished by chest pain that worsens when lying down and improves when sitting, a characteristic not seen in Takotsubo syndrome. Additionally, acute pericarditis often occurs as a complication of an infectious disease, leading to symptoms such as fever and other signs of inflammation.
- Gastroesophageal reflux
Pain associated with gastroesophageal reflux typically develops gradually and is characterized by a burning sensation localized in the central part of the chest. This discomfort is often accompanied by symptoms such as heartburn, nausea, and a sour taste in the mouth, all of which typically alleviate after taking antacids. Unlike Takotsubo syndrome, dyspeptic symptoms are not a hallmark feature of gastroesophageal reflux.
- Gastric ulcer disease
In peptic ulcer disease, pain is frequently localized behind the sternum or in the epigastrium, typically occurring approximately 40 minutes after eating. This discomfort tends to diminish or disappear following the administration of antacids and is often accompanied by symptoms such as nausea and a sour taste in the mouth. Such a pain pattern is not characteristic of Takotsubo syndrome.
- Diseases of the biliary tract
These conditions are typified by the emergence of dull pain behind the sternum or in the epigastrium, typically occurring approximately 1 hour after consuming food, particularly fatty or fried fare. This discomfort is often coupled with nausea, the urge to vomit, and a bitter taste in the mouth. Conversely, chest pain in Takotsubo syndrome is not influenced by dietary intake, and dyspeptic symptoms are generally absent.
- Spontaneous pneumothorax
In spontaneous pneumothorax, intense chest pain abruptly arises, exacerbating with deep breathing, and is accompanied by pronounced shortness of breath. The aggravation of chest pain during inhalation is not a characteristic feature of Takotsubo syndrome.
- Diseases of the neuromuscular system and musculoskeletal system
Chest pain resulting from neuromuscular and musculoskeletal system disorders typically worsens with significant body movements such as turning, bending, or raising the arm, a feature not commonly associated with Takotsubo syndrome.
- Pain in herpes zoster
The pain in herpes zoster typically manifests as a constant burning sensation, often preceding the appearance of a characteristic vesicular rash. It may persist for some time after the rash disappears and is localized along the affected nerve pathway.
Learn more about the specific details of detailing chest pain as the main complaint and taking a patient’s medical history regarding chest pain by visiting the following link:
Other causes of shortness of breath:
- Bronchial asthma
Shortness of breath in bronchial asthma typically manifests as attack-like episodes with an expiratory character. It is often accompanied by wheezing, a sensation of chest tightness, and coughing, often resulting in the discharge of a small amount of glassy viscous sputum. These episodes tend to occur in the early morning hours and are typically relieved by the inhalation of a short-acting β2-agonist.
- Chronic obstructive pulmonary disease
Shortness of breath in chronic obstructive pulmonary disease (COPD) typically has a constant and progressive nature. It is often accompanied by a cough productive of mucus or sputum, particularly in the morning upon waking up.
- Pneumonia
Shortness of breath in pneumonia is often accompanied by an elevated body temperature, symptoms of intoxication, cough with productive sputum, and sometimes chest pain.
- Lung tumor
Shortness of breath associated with lung tumors typically exhibits a constant and progressive nature, often accompanied by hemoptysis, chest pain, coughing, and symptoms of tumor intoxication such as fatigue, weakness, weight loss, and loss of appetite.
- Thromboembolism of the pulmonary artery
Shortness of breath associated with pulmonary embolism typically arises suddenly, often without a known cause. It can be so severe that it impedes the patient’s ability to speak. Additionally, it is accompanied by chest pain of a coronary or pleural nature, hemoptysis, dizziness, or even loss of consciousness. Symptoms of deep vein thrombosis of the lower extremities may also be present.
- Arrhythmia
Tachyarrhythmias, particularly atrial fibrillation, frequently manifest with shortness of breath, palpitations, heart irregularities, and other symptoms indicative of hemodynamic impairment, such as sweating, dizziness, and possibly loss of consciousness. Because rhythm disturbances are typically paroxysmal, shortness of breath also tends to occur in episodes.
- Anemia
Severe anemia often presents with shortness of breath exacerbated by minimal physical exertion, accompanied by rapid heartbeat, angina pectoris-like pains, dizziness, pronounced weakness, and increased fatigue.
- Adiposity
Excess weight often leads to shortness of breath due to increased strain on the cardiovascular system, typically manifesting during physical exertion. In cases of significant excess weight, shortness of breath may even occur at rest.
- Panic attack
Shortness of breath is just one of the symptoms experienced during a panic attack. It typically occurs suddenly and is often accompanied by feelings of fear, anxiety, nausea, palpitations, dry mouth, sweating, and dizziness, which can be unexpected and uncontrollable.
- Hyperventilation
Shortness of breath is the primary symptom of hyperventilation syndrome. Patients commonly describe it as a sudden sensation of breathing dissatisfaction and a feeling of air deprivation. Due to the underlying cause of hyperventilation syndrome, shortness of breath is often accompanied by feelings of anxiety, panic, numbness, and tingling.
- Gastroesophageal reflux disease
Shortness of breath is a relatively rare symptom of gastroesophageal reflux disease and arises due to the prolonged exposure of acidic stomach contents to the respiratory tract, typically after eating, while lying down, or when bending forward. Suspect gastroesophageal reflux disease when more specific symptoms are present, such as heartburn, belching, and discomfort when swallowing food.
History of life
- The accuracy of the presence of previously diagnosed cardiovascular diseases in the patient, in particular myocardial infarction, stroke, rhythm disorders, cardiomyopathy, angina pectoris, arterial hypertension
- Find out whether the patient suffers from mental health disorders, such as depression, anxiety, or schizophrenia, which are risk factors for the development of Takotsubo syndrome
- Determine whether the patient has chronic diseases, in particular diabetes, bronchial asthma, and chronic obstructive pulmonary disease, which are risk factors for the development of Takotsubo syndrome
- Determine whether the patient is taking medications that stimulate the sympathetic nervous system (eg, beta 2-adrenergic receptor agonists, alpha 1-adrenergic receptor agonists, serotonin and norepinephrine reuptake inhibitors, epinephrine)
- Determine whether the patient is abusing psychotropic substances (eg, cannabis, cannabinoids)
- Find out whether the menstrual function is preserved; if not, find out the time of menopause and whether the patient is taking hormone replacement therapy
- Check whether the patient has undergone surgery
- Find out if the patient had any injuries, find out how the recovery period went
- Find out whether the patient has a drug intolerance and specify how it manifests itself
- Find out whether the patient has bad habits – drinking alcohol, narcotic substances, smoking
- Find out the family status of the patient, living conditions, and psychological problems in the family; find out if there were any blood relatives of the patient with cardiovascular diseases
- Find out whether the patient works, his profession, conditions, and nature of work, and whether the work is related to physical or psychological overload
Objective examination:
- Assessment of the patient’s general condition (satisfactory, moderate, severe, very severe).
- General examination of the patient:
- Consciousness, the position of the patient, gait, and posture.
- Physique, type of constitution, height, weight, body mass index.
- Skin and visible mucous membranes (color, rash, scars, scratches), elasticity and moisture of the skin, condition of skin derivatives, and development of subcutaneous adipose tissue.
- Pastiness, edema.
- Lymph nodes.
- Muscular system: development of muscles, their tone, presence of atrophy, soreness.
- Joints: examination, palpation, measurement of limbs and joints, determination of the degree of joint mobility.
- Examination of the head, face, and neck with an assessment of the state of the thyroid gland.
- Research of organ systems
- Research of respiratory organs
- Organs of blood circulation.
- Research of digestive organs.
- Examination of the urinary system.
Assess for objects or equipment on or around the patient that may provide useful information about the patient’s medical history and current clinical condition.
It should be noted that physical findings depend on the severity of Takotsubo syndrome.
In patients with a severe course of Takotsubo syndrome, signs of heart failure can be detected, including wet wheezing in the lungs and tachypnea. During auscultation of the heart, tachycardia, an additional pathological third heart sound, as well as a systolic murmur over the apex of the heart due to obstruction of the outflow tract of the left ventricle and mitral regurgitation are often detected. Additionally, patients with Takotsubo syndrome often exhibit a decrease in blood pressure and low pulse pressure.
In patients with a mild course of Takotsubo syndrome, physical findings are typically unchanged.
Assessment of the probability of Takotsubo syndrome
- Assessment of the probability of Takotsubo syndrome
The probability of Takotsubo syndrome is assessed in patients presenting with chest pain and/or shortness of breath in the absence of ST-segment elevation on the ECG, particularly those hospitalized in intensive care units.
The InterTAK (The International Takotsubo Diagnostic Criteria) diagnostic scale is utilized to assess the likelihood of Takotsubo syndrome. A score of >70 points on this scale indicates a high probability (approximately 90%) of Takotsubo syndrome, whereas a sum of points ≤70 points suggests a low or moderate probability.
| Criteria | Points |
| Female gender | 25 |
| Emotional trigger | 24 |
| Physical trigger | 13 |
| Absence of ST segment depression (except AVR) | 12 |
| Psychiatric disorders | 11 |
| Neurological disorders | 9 |
| Prolongation of the corrected QT interval (women > 460 ms, men > 440 ms) | 6 |
With a high probability of Takotsubo syndrome, urgent transthoracic echocardiography is recommended. For cases with a low or moderate probability of Takotsubo syndrome, coronary angiography is recommended. This procedure allows for definitive differentiation between Takotsubo syndrome and acute myocardial infarction.
Laboratory tests
- Clinical blood count with leukocyte formula and calculation of ESR (erythrocyte sedimentation rate)
- Biochemical blood analysis (total protein, creatinine, urea, alanine aminotransferase, aspartate aminotransferase, glucose, alkaline phosphatase, uric acid, bilirubin with fractions)
- Blood electrolytes (K+ and Na+)
- Lipid profile
- Coagulogram
- Blood test for troponin I / T
- Blood test for creatine phosphokinase (CK)
- Blood analysis for brain natriuretic peptide ( BNP ) or the N-terminal precursor of brain natriuretic peptide (NT – pro-BNP )
- Assessment of thyroid gland function (thyroid-stimulating hormone-TSH) (according to indications)
- Urine analysis with sediment microscopy (as indicated)
- Pregnancy test if the patient is of childbearing age (as indicated)
- Clinical blood count with leukocyte formula and calculation of ESR (erythrocyte sedimentation rate)
Clinical blood count, including the leukocyte count and calculation of the erythrocyte sedimentation rate (ESR), is one of the mandatory laboratory tests conducted in routine clinical practice for somatic patients.
- Biochemical blood analysis (total protein, creatinine, urea, alanine aminotransferase, aspartate aminotransferase, glucose, alkaline phosphatase, uric acid, total bilirubin with its fractions)
The biochemical analysis of blood, which includes measurements of total protein, creatinine, urea, alanine aminotransferase (ALT), aspartate aminotransferase (AST), glucose, alkaline phosphatase, uric acid, and total bilirubin with its fractions, is one of the mandatory laboratory examination methods performed in routine clinical practice for somatic patients.
- Blood electrolytes (K+ and Na+)
Blood analysis for electrolytes (potassium and sodium) is a mandatory laboratory method of examination carried out in routine clinical practice for patients with cardiovascular diseases to diagnose electrolyte disorders.
- Lipid profile
Lipid profile is a mandatory laboratory test for adult patients with cardiovascular diseases to diagnose lipid metabolism disorders.
- Coagulogram
Coagulation profile is a mandatory laboratory test for adult patients with cardiovascular diseases to diagnose disorders of the blood coagulation system.
- Blood test for troponin I / T
“Takotsubo syndrome” is a condition characterized by transient myocardial dysfunction, often triggered by emotional or physical stressors. While troponin levels can be elevated in Takotsubo syndrome, the degree of elevation is typically modest compared to that seen in acute myocardial infarction. It’s important to note that the elevation in troponin levels observed in Takotsubo syndrome is often disproportionate to the extent of regional myocardial dysfunction detected on imaging studies such as echocardiography.
- Blood test for creatine phosphokinase (CK)
Creatine phosphokinase (CK) is indeed an early marker of myocardial necrosis. In Takotsubo syndrome, its levels may show a moderate elevation, typically disproportionate to the extent of regional myocardial dysfunction detected on echocardiography.
- Blood analysis for brain natriuretic peptide ( BNP ) or the N-terminal precursor of brain natriuretic peptide (NT–proBNP )
B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) are indeed markers of heart failure. In Takotsubo syndrome, their levels are often significantly elevated due to the overstretching of cardiomyocytes caused by the condition’s hemodynamic stress.
Appointment of instrumental methods of examination
- Electrocardiography
- Transthoracic echocardiography
- Coronarography
- Ventriculography
- MRI of the heart
- CT angiography of coronary arteries
- Electrocardiography
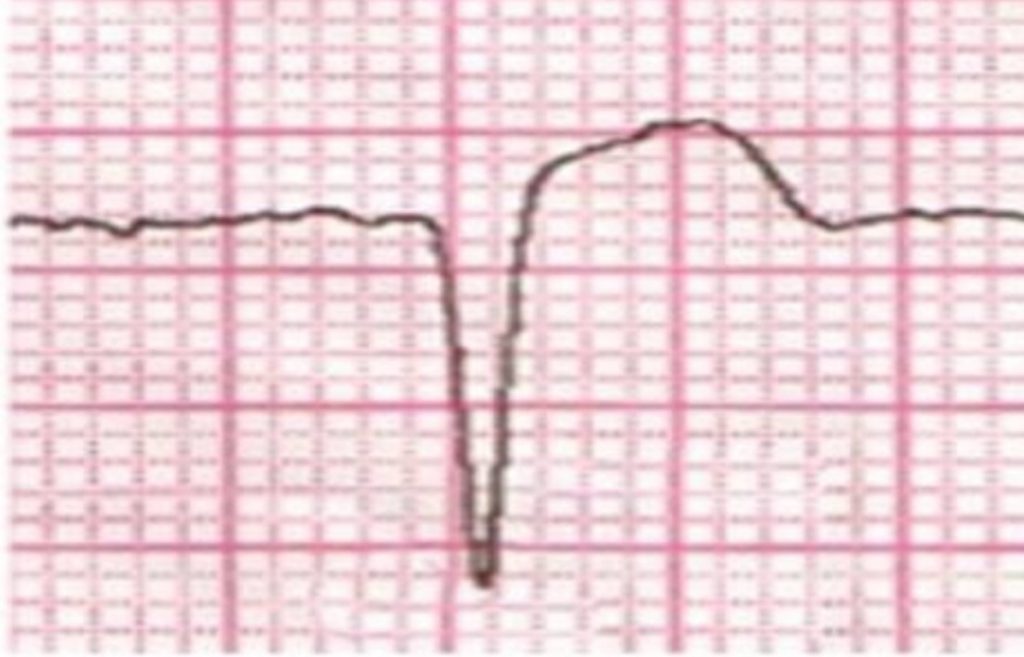
Electrocardiography (ECG) is a mandatory method of examination of patients with suspected Takotsubo syndrome. The most characteristic ECG signs include elevation of the ST segment in the precordial leads, elevation of the ST segment in the AVR lead, diffuse inversion of the T wave, prolongation of the QT interval, rarely depression of the ST segment.
Some experts note that the elevation of the ST segment in the dept. V1-V3 in combination with elevation of the ST segment in the dept. AVR is a characteristic feature of Takotsubo syndrome.
- Transthoracic echocardiography
Transthoracic echocardiography is a mandatory method of examination of patients with suspected Takotsubo syndrome. Moreover, it is diagnostically significant in patients with a high probability of Takotsubo syndrome according to the InterTAK scale.
Echocardiographic signs of Takotsubo syndrome include a decrease in the ejection fraction of the left ventricle, akinesis of the apical segments of the myocardium of the left ventricle in combination with hyperkinesis of the basal part, apical dilatation of the myocardium of the left ventricle, sometimes obstruction of the outflow tract of the left ventricle.
It should be noted that these signs are transitory in nature.
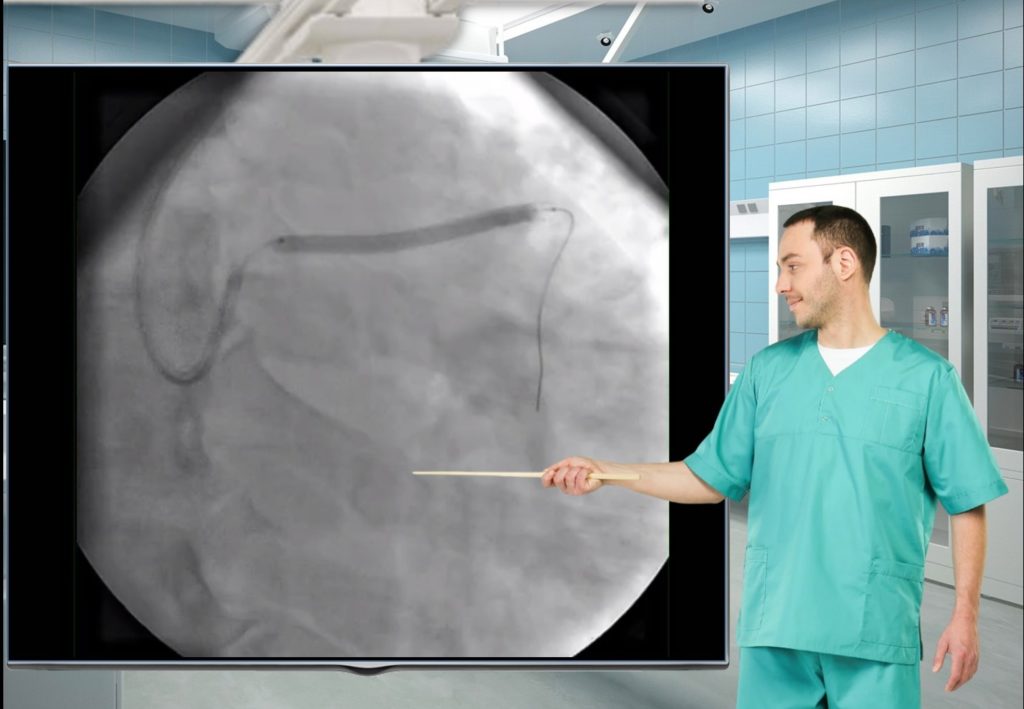
- Coronarography
Coronary angiography indeed serves as a vital diagnostic tool to distinguish Takotsubo syndrome from acute myocardial infarction, particularly in patients with a low or moderate probability of Takotsubo syndrome according to the InterTAK scale.
In individuals with Takotsubo syndrome, coronary angiography typically reveals either normal coronary arteries or coronary arteries with non-obstructive stenosis (defined as stenosis <50%). This absence of significant coronary artery disease further supports the diagnosis of Takotsubo syndrome, helping to differentiate it from acute myocardial infarction.
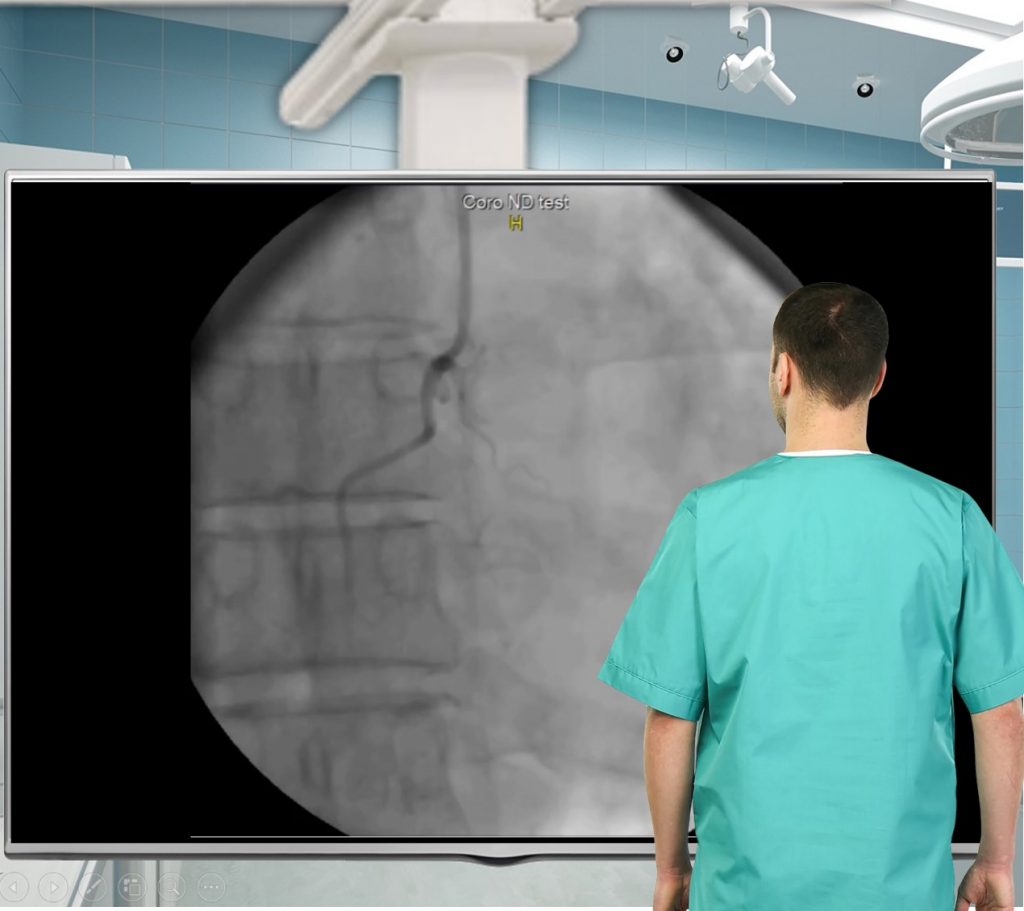
- Ventriculography
Ventriculography provides an assessment of the morphology and function of the left ventricle. In patients with Takotsubo syndrome, transient dysfunction and dilatation of the mid and apical segments of the left ventricle occur, resulting in a heart shape resembling that of an octopus.
- MRI of the heart
MRI of the heart is an informative examination method that allows differentiation between Takotsubo syndrome and myocarditis. Characteristic MRI signs of Takotsubo syndrome include transmural edema in regions with reduced local myocardial contractility and myocardial scarring, while the basal parts of the left ventricle remain normal.
- CT angiography of coronary arteries
CT angiography of the coronary arteries is an alternative examination method for stable patients contraindicated for cardiac MRI. It is performed to rule out significant coronary stenosis.
- Assessment of thyroid gland function (thyroid-stimulating hormone-TSH) (according to indications)
A blood test for thyroid-stimulating hormone is conducted when there is suspicion of thyroid dysfunction, which can contribute to mental health disorders and potentially act as a trigger for the development of Takotsubo syndrome.
- General urine analysis with sediment microscopy (as indicated)
A complete urine analysis with sediment microscopy is conducted when there is suspicion of kidney and/or urinary system damage.
- Pregnancy test if the patient is of childbearing age (as indicated)
It is advisable to conduct a pregnancy test for female patients of childbearing age with Takotsubo syndrome. This helps in selecting appropriate drug therapy tactics, considering that some medications used to treat Takotsubo syndrome are contraindicated during pregnancy due to their teratogenic effects.
Making a clinical diagnosis
- Carrying out differential diagnosis
In clinical practice, it is often necessary to differentiate Takotsubo syndrome from acute coronary syndrome (ACS), acute myocarditis, as well as diseases accompanied by chest pain, in particular, angina pectoris, pulmonary embolism, dissecting aortic aneurysm, acute pericarditis, and others.
Clinical symptoms, objective data, ECG signs of Takotsubo syndrome, and acute coronary syndrome have a lot in common, which causes certain difficulties for differential diagnosis.
Both Takotsubo syndrome and acute coronary syndrome are characterized by complaints of intense radiating chest pain lasting more than 20 minutes and often accompanied by shortness of breath.
Levels of markers of myocardial necrosis, in particular troponin I/T and CK, are increased in both cases, but in Takotsubo syndrome this increase is insignificant compared to patients with acute myocardial infarction.
On the ECG of a patient with Takotsubo syndrome and a patient with ACS, ST-segment elevation and T-wave inversion can often be detected.
Echocardiography of a patient with Takotsubo syndrome and a patient with ACS revealed a decrease in the ejection fraction of the left ventricle and a local violation of myocardial contractility. However, patients with Takotsubo syndrome are characterized by akinesis of the apical segments of the myocardium of the left ventricle in combination with hyperkinesis of the basal part, which leads to apical ballooning of the left ventricle. In addition, these changes are transient and disappear within 3 weeks.
Coronary angiography definitively distinguishes Takotsubo syndrome from acute coronary syndrome. In Takotsubo syndrome, coronary arteries typically appear normal, without evidence of stenosis or hemodynamically insignificant stenosis (<50%). In contrast, acute coronary syndrome is characterized by acute occlusion of the arterial lumen.
Takotsubo syndrome develops in 90% of cases in women over the age of 50, whereas acute myocarditis most often affects young people without gender dominance.
Takotsubo syndrome in most cases is preceded by severe stress, while myocarditis is an infectious disease.
Clinical symptoms such as chest pain, shortness of breath, and palpitations are characteristic of both Takotsubo syndrome and myocarditis.
Blood troponin levels are elevated in both Takotsubo syndrome and myocarditis. However, in Takotsubo syndrome, this increase is insignificant and disproportionate to the area of the affected myocardium, while in myocarditis, troponin is usually significantly increased and correlates with the area of myocardial damage.
The level of brain natriuretic peptide is often elevated in Takotsubo syndrome and is usually elevated in myocarditis.
On the ECG of a patient with cardiomyopathy and myocarditis, changes in the ST segment and inversion of the T wave can often be detected. Unlike Takotsubo syndrome, myocarditis is also characterized by conduction disturbances and arrhythmias.
Echocardiography is important for differential diagnosis. Thus, in Takotsubo syndrome, swelling of the apical segments of the myocardium with intact basal sections is determined, which is not characteristic of myocarditis.
Myocardial edema can often be detected on MRI of the heart in Takotsubo syndrome and myocarditis. However, in the acute stage of Takotsubo syndrome, unlike myocarditis, there is no late accumulation of gadolinium.
Both angina and Takotsubo syndrome are characterized by radiating chest pain. However, in angina, the pain typically lasts up to 20 minutes and subsides with rest or after taking nitrates, whereas in Takotsubo syndrome, the pain persists longer and is not alleviated by nitrates.
The ECG of a patient with angina is usually normal or shows ST-segment depression, whereas patients with Takotsubo syndrome often show ST-segment elevation and T-wave inversion.
In patients with angina pectoris, the levels of markers of myocardial necrosis are normal, while in patients with Takotsubo syndrome, they are elevated.
A coronary angiography of a patient with angina usually shows significant stenosis of the coronary arteries, whereas in Takotsubo syndrome the coronary arteries are either intact or with insignificant stenosis.
Chest pain and shortness of breath are characteristic symptoms of both pulmonary embolism and Takotsubo syndrome. The chest pain in both conditions is anginal in nature.
Blood troponin levels may be mildly elevated in both pulmonary embolism and Takotsubo syndrome.
ECG in patients with pulmonary embolism and Takotsubo syndrome often shows sinus tachycardia, T-wave inversion. Pulmonary embolism is characterized by the classic S I Q III T III pattern, while Takotsubo syndrome is characterized by ST-segment elevation in the precordial leads.
Echocardiography is essential for differential diagnosis. In Takotsubo syndrome, ballooning of the apical segments of the myocardium of the left ventricle with intact basal sections is observed, while in pulmonary artery thromboembolism, akinesia or hypokinesia of the free wall of the right ventricle with preserved contractility of the apex of the right ventricle (McConnell’s sign), 60/60 sign, dilatation and dysfunction of the right ventricle, and acute tricuspid regurgitation may occur.
Patients with a dissecting aortic aneurysm typically describe sudden, excruciating, tearing pain in the chest, which often radiates to the neck, back, and lower limbs and may be migratory. Although the pain in Takotsubo syndrome is intense, it typically does not reach the same level. Physical examination of a patient with a dissecting aortic aneurysm may reveal asymmetry of the pulse and blood pressure in the extremities compared to the other side. In cases where the aortic valve is involved, a diastolic murmur over the aorta and a high pulse pressure may be detected.
On the ECG of a patient with a dissecting aortic aneurysm, as in a patient with Takotsubo syndrome, ST- segment elevation can often be detected, however, in Takotsubo syndrome, ST-segment elevation is visualized in the precordial leads, while in aortic dissection involving the right coronary artery – in leads II, III, AVF.
Echocardiography and chest X-ray have important diagnostic value. On echocardiography and chest X-ray, in the case of aortic arch dissection, dilatation of the affected part of the aorta is revealed, which is not the case with Takotsubo syndrome.
Acute pericarditis is characterized by chest pain that intensifies when lying down and diminishes when sitting up, a feature not typically observed in Takotsubo syndrome. Additionally, patients with acute pericarditis often present with a history or ongoing symptoms of an infectious disease, including fever, respiratory symptoms, and others, which are not commonly associated with Takotsubo syndrome.
Clinical blood analysis of a patient with acute pericarditis reveals signs of an inflammatory process, which is not the case with Takotsubo syndrome.
On the ECG of a patient with acute effusion pericarditis, as in a patient with Takotsubo syndrome, ST -segment elevation, and T-wave inversion can often be detected, however, in Takotsubo syndrome, these changes are visualized in the precordial leads, while in acute pericarditis, ST-segment elevation is diffuse.
Echocardiography is important for differential diagnosis. Thus, in Takotsubo syndrome, ballooning of the apical segments of the myocardium of the left ventricle with intact basal sections is determined, while in pericarditis – thickening and compaction of the pericardial leaves, free fluid in the pericardium, signs of diastolic dysfunction.
- Assessment of diagnostic criteria
Diagnostic criteria are used to establish a clinical diagnosis. Among the existing criteria, the diagnostic criteria of the Mayo Clinic are of the greatest practical importance:
- transient dyskinesia of the middle segments of the left ventricle; local violation of the contractility of the myocardium, which goes beyond the blood supply of one epicardial artery;
- absence of obstructive coronary artery disease or angiographic signs of acute plaque rupture;
- the appearance of new changes on the ECG (elevation of the ST segment and/or inversion of the T wave) or a moderate increase in the level of troponins;
- absence of pheochromocytoma or myocarditis.
In addition to the Mayo Clinic diagnostic criteria, you can use the Takotsubo International Diagnostic Criteria:
- patients with transient dysfunction of the left ventricle in the form of apical, mid-ventricular, basal or focal dilatation; in some cases, the right ventricle is involved in the process; the area of the affected myocardium goes beyond the area of blood supply by one epicardial artery;
- an emotional, physically, or combined trigger preceding the onset of symptoms, but not necessarily;
- neurological disorders (subarachnoid hemorrhage, stroke/transient ischemic attack, convulsions), in particular, pheochromocytoma can serve as a trigger for Takotsubo syndrome;
- the appearance of new changes on the ECG (elevation/depression of the ST segment, inversion of the T wave, prolongation of the QT interval), in rare cases the ECG remains normal;
- a moderate increase in the level of cardiac biomarkers (troponin, CPK) in most cases; a significant increase in the level of BNP and NT-proBNP;
- severe coronary artery disease does not exclude the diagnosis of Takotsubo syndrome;
- absence of signs of infectious myocarditis;
- menopausal women are most often affected.
As well as the criteria of the Heart Failure Association and the European Community:
- transient regional myocardial contractility disorder of the left and right ventricle, which often, but not always, develops as a result of experienced emotional or physical stress;
- the area of the affected myocardium goes beyond the area of blood supply by one epicardial artery and often leads to circular dysfunction of the involved segments of the ventricles;
- absence of obstructive coronary artery disease, including acute plaque rupture, thrombus formation, coronary artery dissection, or other diseases that could explain transient left ventricular dysfunction (eg, hypertrophic cardiomyopathy, viral myocarditis);
- new and reversible changes on the ECG (elevation/depression of the ST segment, inversion of the T wave, prolongation of the QT interval, complete blockade of the left leg of the bundle of His) during the acute phase (3 months);
- significant increase in the level of BNP and NT-proBNP during the acute phase;
- moderate increase in the level of cardiac troponin;
- restoration of the systolic function of the left ventricle, confirmed by MRI of the heart, in dynamics from 3 to 6 months.
- Determination of the anatomical variant
To date, there are several anatomical variants of Takotsubo syndrome: apical or typical (75-80%), mid-left ventricular (10-20%), basal or inverted (5%), biventricular (<0.5%), focal (very rarely).
- Definition of complications
When formulating a clinical diagnosis, it is necessary to indicate the complications that have arisen in the patient, in particular, arrhythmias, heart failure, thromboembolic complications.
- Making of clinical diagnosis
Here is an example of the formulation of the diagnosis in Takotsubo syndrome:
Takotsubo syndrome, apical variant. Ventricular polymorphic polytopic extrasystole, class III according to Laun. ACS-pulmonary edema.
Specialist consultations
- Cardiologist
Given that Takotsubo syndrome is a cardiovascular condition, consulting with a cardiologist for timely diagnosis and appropriate treatment is essential.
- Interventional cardiologist
Considering that Takotsubo syndrome must be differentiated from acute coronary syndrome, it is recommended to perform coronary angiography, which necessitates the involvement of an interventional cardiologist.
- Radiologist
A radiologist is an important member of a multidisciplinary medical team, involved in the implementation of imaging methods of research when Takotsubo syndrome is suspected, particularly magnetic resonance imaging of the heart.
- Psychotherapist
Patients with a confirmed diagnosis of Takotsubo syndrome and mental health disorders are recommended to be referred to a psychotherapist, considering that stress, depression, and anxiety are triggers for the development of Takotsubo syndrome.
- Psychiatrist
Patients with a confirmed diagnosis of Takotsubo syndrome and symptoms of mental disorders are recommended to be referred to a psychotherapist, considering that some of these disorders, including depression, anxiety disorder, and schizophrenia, are factors in the development of Takotsubo syndrome. Additionally, if a depressed patient is taking serotonin and norepinephrine reuptake inhibitors, a psychiatrist should consider replacing them with other drugs, as serotonin and norepinephrine reuptake inhibitors can also trigger the development of Takotsubo syndrome.
- Endocrinologist
Given the established association between hormonal disorders and Takotsubo syndrome, consultation with an endocrinologist is recommended if symptoms of an endocrine disease are present.
- Narcologist
If a patient with suspected Takotsubo syndrome is suspected of using psychotropic substances, they should be referred to a narcologist for consultation. This is because some substances, such as cannabis, cannabinoids, and amphetamines, can provoke the development of Takotsubo syndrome.
- Gynecologist
Considering that Takotsubo syndrome most often occurs in women during menopause, consulting a gynecologist to determine treatment tactics can be beneficial as part of the comprehensive therapy for such patients.
- Doctor of physical and rehabilitation medicine
A physical and rehabilitation medicine physician plays an important role in maintaining the physical well-being of patients with Takotsubo syndrome, assisting them in their recovery process.
Purpose of treatment
- Supportive therapy
- Treatment of complications
- Prevention of relapse
- Supportive therapy
Patients with Takotsubo syndrome require inpatient treatment, the main goal of which is to maintain hemodynamics until normal left ventricular function is restored and to prevent complications. As a rule, supportive treatment lasts several weeks.
Patients with signs of lung congestion, but without hypotension, are prescribed diuretics and nitrates to reduce venous return to the heart. Additionally, ACE inhibitors, ARB II, and beta-blockers are prescribed to help alleviate congestion, reduce myocardial load, and regulate blood pressure.
Patients with unstable hemodynamics require urgent echocardiography to diagnose obstruction of the left ventricular outflow tract. If signs of obstruction are detected, the administration of beta-blockers and IV fluid infusion is recommended, while inotropic drugs are contraindicated. Inotropes such as dopamine, dobutamine, milrinone, and levosimendan are indicated for patients without signs of left ventricular outflow tract obstruction. In severe cases, mechanical circulatory support is necessary, including extracorporeal membrane oxygenation for patients with left ventricular outflow tract obstruction or intra-aortic balloon counterpulsation for patients without obstruction.
An essential aspect of treating patients with Takotsubo syndrome is the prevention of thromboembolic complications, particularly when there is a large area of akinesis or hypokinesis in the myocardium of the left ventricle. To mitigate this risk, anticoagulant therapy is typically prescribed for a duration of 3 months.
- Treatment of complications
The most prevalent complications of Takotsubo syndrome include acute heart failure, left ventricular outflow tract obstruction, arrhythmias, and thromboembolic events.
For acute heart failure, refer to the previously outlined therapy. In cases of arrhythmias or thromboembolic complications, treatment should be administered following established guidelines.
- Prevention of relapse
Considering the high incidence of mental health disorders among Takotsubo syndrome patients, such as depression, anxiety disorders, and substance use, it’s crucial to address these conditions to prevent relapse.
Certain experts advocate for the prolonged use of beta-blockers to mitigate sympathetic nervous system tone, which can serve as adjunctive therapy for anxiety disorders. Retrospective analyses of extensive international registries have shown a beneficial effect of ACE inhibitors, ARBs, and calcium channel antagonists.
Consulting and support:
- Informing the patient about the disease
- Discussion of research results with the patient
- Explanation to the patient of the possible cause of the disease
- Explanation to the patient of possible symptoms that may occur during the disease
- Explanation to the patient of the possible consequences of the disease
- Explaining the available treatment methods, informing the patient about the risks and benefits of different treatment methods
- Answers to the patient’s questions
- Explanation of the scope of monitoring during and after treatment
- Appointment of regular checks and controls to assess the effectiveness of treatment and changes in the patient’s condition
| Inform the patient about the disease | “Mr./Ms…., I’d like to discuss your diagnosis with you. You’ve been diagnosed with Takotsubo syndrome. This condition occurs when the heart temporarily loses its ability to function normally due to severe emotional stress”. |
| Explain to the patient the possible causes of the disease | “There are several factors that can contribute to the development of Takotsubo syndrome. These include emotional stress, mental health disorders, hormonal imbalances, certain medications, genetic predisposition, among others. Emotional stress is often the primary trigger, leading to the release of large amounts of catecholamines such as adrenaline and norepinephrine. These chemicals can constrict blood vessels and disrupt normal heart function. To determine the exact cause of Takotsubo syndrome, further examinations will be necessary. Once we identify the underlying cause, we can determine the most appropriate treatment approach.” |
| Inform the patient of the symptoms that may occur with the identified disease | “The symptoms of Takotsubo syndrome can resemble those of a heart attack. Typically, patients experience intense chest pain that persists even after taking nitrates, along with shortness of breath. In severe cases, patients may also develop rhythm disturbances and thromboembolic complications.” |
| Discuss the results of the examinations with the patient | “Mr./Ms. [Last Name], I’d like to discuss the results of your examinations with you. During the electrocardiography, we observed changes similar to those seen in myocardial infarction. However, further examinations did not confirm this diagnosis. Coronary angiography showed no evidence of thrombosis in the heart arteries, which would typically indicate a myocardial infarction. Additionally, echocardiography revealed transient heart contractility, characteristic of Takotsubo syndrome rather than myocardial infarction. To confirm the diagnosis, we performed ventriculography, which revealed changes in heart shape during contraction typical of Takotsubo syndrome. Do you have any questions or concerns about what I’ve just explained?” |
| Explain to the patient the possible consequences of the disease | “The prognosis for Takotsubo syndrome is generally favorable, as heart contractility issues are temporary and typically resolve within 2-3 weeks. However, during this period, it’s crucial to adhere to the doctor’s recommendations aimed at reducing strain on the weakened heart and preventing complications.” |
| Educate the patient about available treatments | “I’d like to discuss the available treatment methods for Takotsubo syndrome, aiming primarily at maintaining blood circulation until the heart’s normal function is restored. The choice of treatment method depends on the severity of the syndrome. Patients without signs of heart failure typically receive beta-blockers, angiotensin-converting enzyme inhibitors, or angiotensin II receptor blockers. For those exhibiting lung congestion without low blood pressure, diuretics and nitrates are prescribed to alleviate congestion, reduce cardiac workload, and regulate blood pressure. If there’s unstable circulation, intravenous solutions and/or inotropic drugs may be administered to enhance myocardial contractility. In cases where drug therapy proves ineffective, mechanical circulatory support using various devices may be employed“. |
| Help the patient understand the risks and benefits of different treatments | “Although the medications used to treat Takotsubo syndrome are well-studied, effective, and generally safe, there is a possibility of side effects with therapy. However, I want to assure you that we will take every precaution to minimize these risks.” |
| Answer the patient’s questions | “If you have any further questions regarding the causes of the disease, its symptoms, diagnosis, or treatment, please feel free to ask. It’s crucial that you understand what’s happening and what steps we’ll be taking next.” |
| Provide an explanation of the extent of monitoring during and after treatment | “Monitoring, or observing the main parameters of your body, is crucial for timely assessment of your condition, correction of detected changes, and evaluating the effectiveness of treatment. During monitoring, we will carefully observe your general condition, blood oxygen saturation level, blood pressure, heart rate, and myocardial contractility. Pulse oximetry is performed to determine the level of blood oxygen saturation. A special pulse oximeter device will be worn on your finger to constantly monitor the oxygen level in your blood. Blood pressure monitoring allows us to assess how well your heart is functioning and make corrections if there is a significant decrease or increase in blood pressure. We will use electrocardiography to evaluate heart rhythm by placing special electrodes on the front chest wall to record the electrical activity of your heart. This will enable us to monitor the effect of the treatment. To assess myocardial contractility, we will repeat echocardiography.” |
| Schedule regular check-ups and follow-up to assess the effectiveness of treatment and changes in the patient’s condition | “After discharge from the hospital, it’s important to monitor your well-being and avoid emotional and physical stress. If you experience anxiety, depression, or other mental health disorders, it’s advisable to consult a psychotherapist to determine the appropriate course of action. Your emotional well-being is crucial to prevent the recurrence of Takotsubo syndrome.” |
End of consultation
- Summarize the data and ask the patient if anything important has been missed
- Inform the patient about further tactics
Hospitalization to a specialized cardiology hospital is recommended for a comprehensive examination and selection of optimal treatment tactics. Obtain the patient’s Informed Voluntary Consent for diagnosis and treatment, and agree to the Patient’s Informed Voluntary Consent for processing personal data.
- Thank the patient
- Dispose of PPE properly and wash hands
Key communication skills
- Active listening
- Summing up
- Selection of indicative signs
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Acute Pulmonary Edema: Emergency Care Algorithm – Should We Remove or Redistribute the Fluid?
Case Presentation: A 64-year-old man was transported to the emergency department by ambulance due to…
Takotsubo syndrome
Takotsubo syndrome is a condition characterized by the sudden onset of acute, transient (lasting up…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…
Symptomatic bradycardia
Symptomatic bradycardia occurs when the heart rate drops below 50 beats per minute. Most often,…
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
SAVED VTE Score
SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…