Acute Pulmonary Edema: Emergency Care Algorithm – Should We Remove or Redistribute the Fluid?

Case Presentation:
A 64-year-old man was transported to the emergency department by ambulance due to a progressively worsening shortness of breath over the past two weeks. He also noticed swelling in his legs. The patient reports feeling breathless when climbing stairs or walking more than two blocks. Approximately one month ago, he suffered an ST-elevation myocardial infarction, which required the implantation of a stent in the left anterior descending artery.
On physical examination, elevated jugular venous pressure was noted, along with bilateral lower extremity edema. Lung auscultation revealed bilateral crepitation in the basal regions. A chest X-ray showed bilateral pleural effusion and the presence of Kerley B lines.
Pulmonary edema
Acute pulmonary edema is a life-threatening emergency that requires immediate medical intervention. It is characterized by secondary shortness of breath and hypoxia, resulting from fluid accumulation in the lungs, which disrupts gas exchange.
Acute heart failure (HF) typically manifests as “acute decompensated heart failure” (ADHF), secondary chronic heart failure (CHF), or de novo heart failure. The most severe complications of acute heart failure are acute pulmonary edema and cardiogenic shock. According to the EuroHeart Failure Survey II, 37% of patients hospitalized with heart failure presented with de novo acute heart failure, and 16% had acute pulmonary edema.
Acute pulmonary edema has a high mortality rate, requiring urgent care and often hospitalization. The one-year mortality rate for patients hospitalized with acute pulmonary edema is as high as 40%.
The most common causes of acute pulmonary edema include myocardial ischemia, arrhythmias (e.g., atrial fibrillation), acute valvular dysfunction, and fluid overload. Other contributing factors can include pulmonary embolism, anemia, and renal artery stenosis. Non-adherence to treatment plans and adverse drug effects may also precipitate pulmonary edema.
General practitioners are typically familiar with the classic presentation of acute pulmonary edema—severe dyspnea, distress, pallor, sweating, tachycardia, and decreased peripheral perfusion. However, in primary care settings, the clinical manifestations of acute heart failure may be less pronounced or atypical (e.g., delirium or falls in the elderly), making timely diagnosis more challenging.
Pulmonary edema is the accumulation of fluid in the interstitial space and air spaces of the alveoli, impairing normal gas exchange.
Types of Pulmonary Edema
- Cardiogenic Pulmonary Edema
This occurs due to a sharp increase in left ventricular filling pressure and left atrial volume, leading to increased pulmonary capillary pressure.- Atrial Outflow Obstruction
Pulmonary edema can result from mitral stenosis or, more rarely, from conditions like atrial myxoma, thrombosis of a prosthetic valve, or a congenital membrane in the left atrium (e.g., cor triatriatum). Mitral stenosis, often a consequence of rheumatic fever, gradually causes pulmonary edema. Other factors commonly accompany mitral stenosis in acute pulmonary edema, such as reduced left ventricular filling caused by tachycardia in arrhythmias (e.g., atrial fibrillation) or fever. - Causes of Left Ventricular Dysfunction:
- Ischemic heart disease
- Hypertension
- Acute and chronic heart valve disease (e.g., aortic stenosis, aortic regurgitation, mitral regurgitation)
- Dilated cardiomyopathy
- Metabolic conditions (e.g., hypothyroidism)
- Myocarditis
- Myocardial toxins (e.g., alcohol, cocaine, chemotherapeutic agents such as doxorubicin, trastuzumab)
- Ventricular hypertrophy
- Outflow obstruction
- Left ventricular diastolic dysfunction (ischemia and infarction can cause diastolic dysfunction in addition to systolic dysfunction). Similarly, myocardial injury can cause systolic or diastolic dysfunction.
- Arrhythmias
Tachysystolic atrial fibrillation and ventricular tachycardia can precipitate pulmonary edema. - Non-Compliance with Dietary or Medication Guidelines
Failure to adhere to dietary salt restrictions or prescribed medications (e.g., diuretics) can lead to fluid retention and pulmonary edema.
- Atrial Outflow Obstruction
- Non-Cardiogenic Pulmonary Edema
Pulmonary edema with normal pulmonary artery pressure (≤ 18 mm Hg).- Causes include:
- Acute respiratory distress syndrome (ARDS)
- High-altitude pulmonary edema (HAPE)
- Opioid overdose
- Hypoxia, shortness of breath, and dry cough due to altitude exposure in cases of altitude sickness.
- Causes include:
Symptoms
- Sudden onset of severe shortness of breath.
- Anxiety and a feeling of drowning.
- Profuse sweating.
- Patients with a gradual onset of symptoms (e.g., over 24 hours) often report dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea.
- Cough is a common symptom. Pink, frothy sputum may occur in severe cases. Occasionally, hoarseness (Ortner’s sign) can result from compression or recurrent paralysis of the laryngeal nerve by an enlarged left atrium, as seen with mitral stenosis.
- Chest pain should raise suspicion for acute ischemia, myocardial infarction, or aortic dissection with acute aortic regurgitation causing pulmonary edema.
Physical Examination
- Tachypnea and tachycardia are often present. Patients may adopt an upright position (orthopnea) and become agitated or confused. They usually appear anxious, with profuse sweating.
- Hypertension is commonly seen in the hyperadrenergic state.
Hypotension indicates severe left ventricular (LV) systolic dysfunction and the possibility of cardiogenic shock. - Cool extremities may signal low cardiac output and poor peripheral perfusion.
- Lung auscultation typically reveals fine crackles (rales), often starting in the lung bases. As the condition worsens, the crackles progress toward the upper lung fields. Wheezing may also be present. Jugular venous distention may indicate increased right heart pressures.
- Heart auscultation can aid in diagnosing acute valvular disorders that manifest with pulmonary edema:
- Aortic stenosis is associated with a crescendo-decrescendo systolic murmur, best heard at the upper sternal border, radiating to the carotid arteries.
- Acute aortic regurgitation presents with a short, soft diastolic murmur.
- Acute mitral regurgitation produces a loud systolic murmur, best heard at the apex or lower left sternal border. In the context of ischemic heart disease, this may indicate acute myocardial infarction with rupture of the mitral valve chordae.
- Rust-colored sputum may result from ruptured pulmonary capillaries due to increased hydrostatic pressure.
- Pallor or mottled skin can result from peripheral vasoconstriction, low cardiac output, and blood shunting to the central circulation in patients with poor LV function and increased sympathetic tone. Mottled skin is an independent predictor of increased in-hospital mortality.
- In patients with concomitant right ventricular failure, hepatomegaly, hepatojugular reflux, and peripheral edema may be observed.
- Severe acute pulmonary edema may be associated with altered mental status, often due to hypoxia or hypercapnia. Although acute pulmonary edema is typically associated with hypocapnia, hypercapnia and respiratory acidosis can occur in patients with severe or underlying chronic obstructive pulmonary disease (COPD).
Differential Diagnosis
- Pneumonia
- Diffuse opacification of lung fields due to atelectasis without fluid accumulation
Additional Examination Methods
- Chest X-ray
Signs of increased left atrial pressure, Kerley B lines, and pleural effusion. - Echocardiography
- Reduced or preserved left ventricular ejection fraction (LVEF)
- Valvular abnormalities, chordal or papillary muscle rupture
- Mitral regurgitation
- Aortic stenosis
Causes of Acute Pulmonary Edema
Cardiogenic pulmonary edema must be distinguished from pulmonary edema caused by damage to the alveolar-capillary membrane, which can result from various etiologies. Damage to this barrier may occur in several direct lung injuries (such as pneumonia, aspiration pneumonitis, toxin inhalation, radiation exposure, drowning, or fat embolism) as well as in indirect lung injuries (such as sepsis, shock, multiple blood transfusions, acute pancreatitis, or anaphylactic shock).
The most common cause of heart failure is myocardial dysfunction, which can arise due to one or more of the following factors:
- Hypertension (present in over 60% of patients with heart failure)
- Ischemic heart disease (present in over 50% of patients with heart failure)
- Idiopathic dilated cardiomyopathy (seen in approximately 10% of patients with heart failure)
- Diabetes mellitus
- Excessive alcohol consumption
- Obesity
- Drug toxicity
Other cardiac causes of heart failure include arrhythmias, valvular dysfunction, and pericardial disease.
Non-cardiac causes of heart failure include hypovolemia (due to dehydration or hemorrhage), pulmonary embolism, and conditions associated with increased cardiac output (such as anemia, sepsis, and thyrotoxicosis).
Cardiogenic pulmonary edema is defined as pulmonary edema caused by elevated capillary hydrostatic pressure, which is secondary to increased pulmonary venous pressure. It reflects the accumulation of low-protein fluid in the pulmonary interstitium and alveoli as a result of cardiac dysfunction.
Stages of Development of Pulmonary Edema
The progression of fluid accumulation in acute pulmonary edema can be described in three physiological stages:
Stage 1
In the initial stage, increased pressure in the pulmonary artery leads to the stretching and opening of small pulmonary vessels. At this stage, gas exchange is not significantly impaired and may even slightly improve. This is due to the redistribution of blood flow within the lungs, enhancing perfusion in certain areas.
Stage 2
In stage 2, fluid and colloids begin to move from the pulmonary capillaries into the pulmonary interstitium. Initially, the lymphatic system compensates by increasing lymphatic outflow to efficiently remove the excess fluid. However, continued fluid filtration can overwhelm the drainage capacity of the lymphatic system. Fluid first accumulates in the compliant interstitial compartments, especially around large vessels in dependent zones (such as the perivascular tissue).
At this stage, the accumulation of fluid in the interstitium can start to affect the function of small airways, leading to mild hypoxemia. However, the hypoxemia is usually not severe enough to cause significant tachypnea. Any tachypnea that does occur is mainly due to the stimulation of juxtapulmonary capillary (J-type) receptors, which are unmyelinated nerve endings near the alveoli. These receptors are involved in reflexes that regulate respiration and heart rate.
Stage 3
In the final stage, as fluid filtration continues and the loose interstitial space becomes filled, excess fluid crosses into the alveolar spaces. The interstitial space can accommodate up to approximately 500 mL of fluid. Once the interstitial capacity is exceeded, fluid moves across the alveolar epithelium into the alveoli. At this stage, gas exchange is noticeably impaired, vital capacity and other lung volumes are significantly reduced, and hypoxemia becomes more pronounced. This is when patients typically experience more severe respiratory distress and worsening oxygenation.
Diagnostics
Laboratory tests and imaging are essential for evaluating patients with cardiogenic pulmonary edema. The following diagnostic tools are commonly used:
Complete Blood Count (CBC)
A CBC is useful for detecting severe anemia and may reveal signs of sepsis or infection, particularly if there is a significantly elevated white blood cell count.
Serum Electrolytes
Measuring serum electrolytes is important because patients with chronic heart failure often take diuretics, making them prone to electrolyte imbalances, especially hypokalemia and hypomagnesemia. Patients with chronic renal failure are at high risk for hyperkalemia, particularly if they are not undergoing regular hemodialysis.
Blood Urea Nitrogen (BUN) and Creatinine Levels
These tests assess kidney function, which is crucial for evaluating the patient’s potential response to diuretics and identifying any underlying renal failure.
Pulse Oximetry
Pulse oximetry is used to assess hypoxia, providing insight into the severity of acute pulmonary edema. It is also helpful for monitoring the patient’s response to supplemental oxygen therapy and other treatments.
Arterial Blood Gas (ABG) Analysis
ABG analysis offers a more precise measurement of oxygen saturation compared to pulse oximetry. While the decision to initiate mechanical ventilation is usually based on clinical findings, ABG results may be considered in more complex cases.
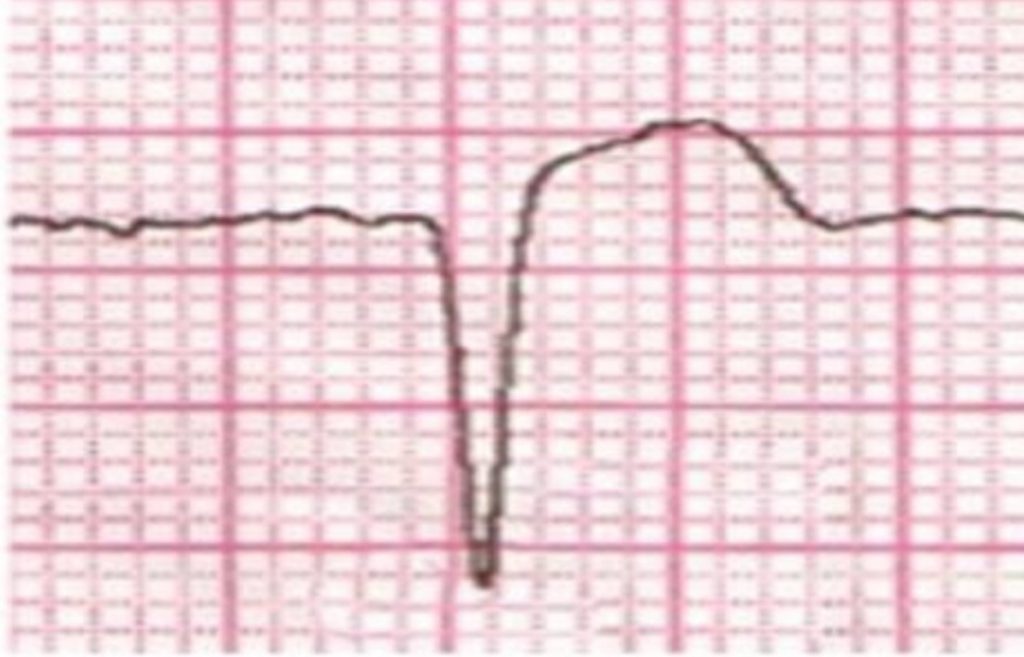
Electrocardiography (ECG)
An ECG can detect acute tachyarrhythmias or bradyarrhythmias, as well as signs of acute myocardial ischemia or myocardial infarction, which may be contributing factors to pulmonary edema.
Chest Radiography (X-ray)
A chest X-ray helps differentiate cardiogenic pulmonary edema from other pulmonary causes of severe dyspnea. Key features of cardiogenic pulmonary edema on a chest X-ray include:
- Enlarged heart (cardiomegaly)
- Redistribution of blood flow
- Kerley B lines (indicative of interstitial edema)
- Edema in the basal parts of the lungs (contrasted with diffuse edema)
- Absence of air bronchograms
- Presence of pleural effusion, particularly bilateral and symmetrical, which is more common in acute presentations of chronic heart failure
Table: Differential Diagnosis of Acute Shortness of Breath and Causes of Acute Pulmonary Edema
| Category | Conditions |
|---|---|
| Primary Causes of Breathing Disorders | – Exacerbation of chronic obstructive pulmonary disease (COPD) – Acute asthma – Pneumothorax – Pneumonia |
| Primary Cardiac Causes | – Acute coronary syndrome / myocardial infarction – Arrhythmia – Pericarditis – Acute valve dysfunction (e.g., aortic stenosis, mitral regurgitation) – Endocarditis |
| Fluid Overload | – Anaphylaxis – Hypervolemia due to excessive fluid intake or renal failure – Medication effects (e.g., NSAIDs, non-dihydropyridine calcium channel blockers such as verapamil and diltiazem) |
| Non-Cardiogenic Causes of Acute Pulmonary Edema | – Drowning – Laryngospasm / upper airway obstruction – Toxic inhalation |
| Pulmonary Embolism | – Acute pulmonary embolism with sudden onset of dyspnea |
| Acute Renal Failure | – Fluid overload and electrolyte imbalances associated with acute renal failure |
| Conditions with Increased Cardiac Output | – Septicemia – Anemia – Thyrotoxicosis |
Table: Differential Diagnosis of Acute Pulmonary Edema
| Condition | Key Features |
|---|---|
| Cardiogenic Pulmonary Edema | – Increased pulmonary capillary pressure |
| – Symptoms: shortness of breath, orthopnea, cough, anxiety | |
| – Signs: crackles on auscultation, jugular venous distension | |
| Pneumonia | – Symptoms: cough, fever, chills, pleuritic chest pain |
| – Chest X-ray: localized infiltrates, air bronchograms | |
| Acute Respiratory Distress Syndrome (ARDS) | – Symptoms: severe dyspnea, rapid onset |
| – Chest X-ray: bilateral infiltrates, often with a history of trauma or sepsis | |
| Chronic Obstructive Pulmonary Disease (COPD) Exacerbation | – Symptoms: increased sputum production, wheezing, prolonged expiratory phase |
| – History of smoking or prior lung disease | |
| Pulmonary Embolism | – Symptoms: sudden onset of dyspnea, chest pain, hemoptysis |
| – Risk factors: recent surgery, prolonged immobility | |
| – Chest X-ray: may be normal; CT pulmonary angiography is diagnostic | |
| Acute Kidney Injury (AKI) | – Symptoms: fluid overload, electrolyte imbalances |
| – Elevated BUN and creatinine levels | |
| Anaphylaxis | – Symptoms: urticaria, angioedema, hypotension, wheezing |
| – History of exposure to allergens |
Echocardiography
Bedside echocardiography in patients with decompensated congestive heart failure (CHF) is an essential diagnostic tool for determining the etiology of pulmonary edema. This imaging modality can assess left ventricular (LV) systolic and diastolic function, as well as evaluate valvular function and pericardial disease.
The identification of new wall motion abnormalities may suggest an acute myocardial infarction. Echocardiography is particularly valuable in diagnosing the mechanical causes of pulmonary edema, including the following conditions:
- Acute rupture of the papillary muscle
- Acute ventricular septal defect
- Cardiac tamponade
- LV rupture
- Valve vegetation leading to acute severe mitral or aortic regurgitation
Treatment
The management of both acute heart failure and acute pulmonary edema is primarily based on clinical experience rather than randomized controlled trials.
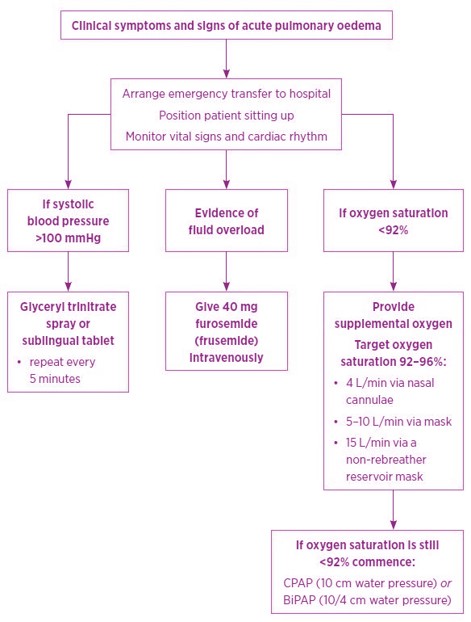
The algorithm for providing medical care can be conditionally divided into two stages:
- Pre-Hospital Care: This involves immediate assistance to stabilize the patient before they reach the hospital.
- Hospital Care: This stage focuses on comprehensive treatment and monitoring of the patient after admission.
While there are various clinical guidelines for treating acute pulmonary edema, the general principles across these guidelines remain consistent. The goals of therapy for acute pulmonary edema include:
- Improving oxygenation
- Maintaining adequate blood pressure to ensure perfusion of vital organs
- Reducing excess extracellular fluid
Additionally, it is crucial to address the underlying cause of the condition or mitigate its impact on the patient’s status.
Evaluation of a Patient with Acute Pulmonary Edema
Entry Level
- Quickly alert relevant personnel (doctors, nurses, clinic staff).
- Initiate oxygen therapy.
- Establish intravenous access.
- Start treatment during patient examination.
Patient History
- Previous cardiorespiratory complaints (e.g., nocturnal dyspnea, orthopnea).
- List of medications taken.
Objective Review
- Vital Signs:
- Temperature
- Pulse (frequency, rhythm)
- Blood pressure
- Respiratory rate (frequency, character)
- Oxygen saturation
- Targeted Cardiorespiratory Examination:
- Skin color
- Sweating
- Jugular venous pulse
- Apical impulse (displacement, load)
- Heart sounds (e.g., gallop rhythm)
- Murmurs (e.g., mitral regurgitation, aortic stenosis)
- Peripheral perfusion and edema
- Auscultation for crepitations and wheezing
Monitoring
- Blood pressure
- ECG monitoring (lead II), if possible
- Oxygen saturation
- Automated external defibrillator on standby
- Urinary catheter
Additional Research Methods (Depending on Availability)
- 12-lead ECG
- Chest X-ray
- Laboratory tests (if available):
- Troponin
- Natriuretic peptide (BNP)
- Other tests: blood urea nitrogen, electrolyte levels, arterial blood gases
- Echocardiogram at the earliest opportunity (depending on patient stability and availability)
Drugs Used in Treatment
The medications commonly used in the management of acute pulmonary edema include nitrates, diuretics, morphine, and inotropes. Some patients may also require ventilatory support.
Strongest Evidence
Nitrates and noninvasive ventilation have the strongest evidence for efficacy in treating acute pulmonary edema. Diuretics are indicated only for patients with fluid overload; furosemide should be administered slowly via intravenous infusion. The most common causes of cardiogenic pulmonary edema include excessive venous return (fluid overload), increased systemic vascular resistance (e.g., after exercise), and left ventricular dysfunction, which can involve contractility disorders, rhythm disturbances, and frequency issues.
Continuous use of morphine is not recommended due to its potential adverse effects. Oxygen should be administered only in cases of hypoxemia.
Inotropic agents should be initiated only when hypotension is present with reduced organ perfusion. In such cases, dobutamine is usually the first-line treatment.
Table. Treatment of acute pulmonary edema
| Therapy / Tactics | Dosage | Clarification |
|---|---|---|
| Position | – Vertical position of the patient while sitting. | |
| – Lying on the back if unconscious or in cardiogenic shock. | ||
| Oxygen (corrects hypoxemia) | 10–15 L/min via mask with reservoir bag. | – Once stable, reduce to 2–6 L/min via nasal cannula or 5–10 L/min via mask. |
| – COPD patients should ideally receive controlled oxygen therapy via mask (flow rate 4 L/min). | ||
| – Titrate to oxygen saturation of 94–96% (non-COPD) or 88–92% (COPD). | ||
| Glyceryl Trinitrate (venodilator, reduces preload) | 400 mcg sublingually every 5 minutes (up to three doses). | – Maintain systolic blood pressure above 100 mm Hg. |
| Intravenous infusion starting at 10 mcg/min. | – Double the infusion rate every 5 minutes according to clinical response (maintain SBP above 90 mm Hg). | |
| – Contraindicated within 48 hours after using phosphodiesterase 5 inhibitors. | ||
| Positive Airway Pressure Support | CPAP: Constant positive pressure of 10 cm H2O. | – BiPAP: Inspiratory pressure of 15 cm H2O, expiratory pressure of 5 cm H2O to prevent alveolar collapse. |
| – Contraindicated if: SBP <90 mm Hg; loss of consciousness. | ||
| – Clinical improvement can occur within 10 minutes; duration of use depends on effectiveness and tolerability. | ||
| Frusemide (loop diuretic, reduces congestion) | 20–80 mg IV bolus. | – Followed by IV infusion at 5–10 mg/h (total dose <100 mg during the first 6 hours and <240 mg during the first 24 hours). |
| – Consider repeating the bolus dose in 30–60 minutes if no clinical improvement is observed. | ||
| – High risk of hypovolemia and negative hemodynamic effects; avoid unless there is evidence of fluid overload. | ||
| Morphine | 1–2 mg IV. | – Does not improve pulmonary edema and is associated with an unfavorable prognosis. |
| – Use according to individual indications. | ||
| Other Medications | – Low Molecular Weight Heparin (Prophylaxis of venous thromboembolism): Enoxaparin 40 mg/day. Start if there is risk. | |
| – Digoxin: 500 mcg IV (over 5 or more minutes). Only for patients with tachysystolic atrial fibrillation who have not previously received digoxin. | ||
| – Spironolactone: 25–50 mg orally. Consider in cases of fluid overload with poor response to IV furosemide. | ||
| Other Methods of Therapy (ICU) | – Adrenaline infusion. | |
| – Vasopressin antagonists (conivaptan, tolvaptan). | ||
| – Vasodilators (sodium nitroprusside). | ||
| – Inotropes: for cardiogenic shock or hypoperfusion with BP <90 mmHg (dobutamine, dopamine). | ||
| – Phosphodiesterase inhibitors (milrinone, enoximone). | ||
| – Ultrafiltration. | ||
| – Mechanical Support (e.g., intra-aortic balloon counterpulsation) in cardiogenic shock. |
Nitrates
The mechanism of action of nitrates involves the relaxation of smooth muscle, leading to the dilation of veins and a consequent reduction in preload at low doses. At higher doses, nitrates also cause the dilation of arterioles, which results in decreased preload and blood pressure. In the coronary arteries, this dilation enhances coronary blood flow. Collectively, these actions improve oxygenation and decrease the workload on the heart.
In clinical practice, nitrates are often prescribed sublingually. Intravenous infusions of nitroglycerin are also used, as this route allows for rapid onset of action and precise dose titration.
Advantages of using nitro preparations for acute pulmonary edema:
- Fast and reliable reduction of preload.
- Medium to high doses decrease systemic vascular resistance (afterload), helping to maintain or improve stroke volume and cardiac output.
- Various routes of administration: sublingual and intravenous.
- Short duration of action and rapid metabolism (approximately 60 mcg per minute).
Therefore, nitroglycerin is considered a first-line medication during both the pre-hospital and early hospital stages for patients with acute pulmonary edema.
Contraindications: The use of nitrates should be avoided if the patient has taken phosphodiesterase inhibitors (e.g., sildenafil, vardenafil, tadalafil) within the last 48 hours, as these medications are commonly prescribed for erectile dysfunction and pulmonary hypertension. Additionally, avoid the intravenous administration of eprostenol or treprostinil, which are used in the treatment of pulmonary hypertension.
Nitrates are also not recommended for patients with myocardial infarction of the inferior wall or for those suspected of having an ST-segment elevation myocardial infarction affecting the right ventricle, as these patients require adequate preload for the right ventricle. Moreover, nitrates should not be used in patients with aortic stenosis, hypotension, or acute mitral insufficiency.
Recommended Modes of Use of Nitro Preparations
| Drug/Mode of Administration | Dosage | Frequency | Maximum Dose |
|---|---|---|---|
| Glyceryl Trinitrate Spray | 400 micrograms (2 sprays) | Repeat every 5 minutes | 1200 micrograms |
| Sublingual Tablet of Glyceryl Trinitrate | 300-600 micrograms | Repeat every 5 minutes | 1800 micrograms |
| Intravenous Infusion of Glyceryl Trinitrate | 5–10 micrograms/min | Doubling every 5 minutes if SBP is stable | 200 micrograms/min |
In the conducted studies, a high efficacy of sublingual administration of nitroglycerin at a dose of 0.4 mg every 5 minutes was demonstrated until the onset of a pronounced clinical effect. The administration of the drug according to this regimen is recognized as equivalent to intravenous administration of nitroglycerin at a rate of 60 μg/min.
Diuretics
The use of furosemide is not recommended at the pre-hospital stage. Pulmonary edema is more commonly related to volume distribution rather than volume overload; therefore, furosemide does not provide improvement in most patients.
The administration of furosemide can lead to increased afterload due to vasoconstriction and decreased renal blood flow. In some patients, this may result in a significant drop in cardiac output and systemic pressure, potentially increasing the risk of fatal arrhythmias.
An incorrect diagnosis of chronic congestive heart failure, coupled with excessive diuresis, can lead to complications and fatalities. This is because the use of furosemide:
- Reduces preload through increased diuresis, but has a delayed effect.
- Causes an initial negative hemodynamic response, characterized by increased systemic vascular resistance, decreased stroke volume, and reduced cardiac output.
- Can be detrimental when administered to patients with severe cardiogenic pulmonary edema in the first minutes of medical assistance.
Diuretics are indicated only for patients who exhibit signs of fluid overload. Intravenous administration of furosemide in doses of 40 to 80 mg is preferred. Higher doses may be required for patients already on oral diuretics or those with chronic kidney disease. The initial bolus can be administered slowly via intravenous infusion and repeated after 20 minutes if necessary. Following the bolus, a continuous intravenous infusion can be considered, starting at a rate of 5–10 mg per hour. Higher doses have been associated with better results in alleviating dyspnea but also with worsening renal function and increased hospitalizations in intensive care units. However, this association likely reflects the presence of more severe comorbidities and underlying diseases that contribute to the development of acute pulmonary edema. An indwelling urinary catheter should be placed to monitor urine output volume.
Recommended Dosage Regimens of Furosemide
| Drug, Mode of Administration | Dosage | Frequency |
|---|---|---|
| Slow intravenous bolus | 4 mg/min | Repeat after 20 minutes if necessary |
| Normal kidney function: 40–80 mg | 40–80 mg | – |
| Kidney failure or severe heart failure | Up to 160–200 mg | – |
| Chronic use of loop diuretics | Initial IV dose equal to oral maintenance dose* Titrate in response to clinical need | |
| Intravenous infusion | 5–10 mg per hour | Continuously |
*The bioavailability of the oral preparation of furosemide (frusemide) is approximately half that of the intravenous form.
Morphine
Morphine was traditionally part of the treatment regimen for acute pulmonary edema due to its ability to reduce shortness of breath. It also lowers sympathetic nervous system activity, which may help alleviate anxiety and distress associated with dyspnea.
However, the use of morphine carries several side effects, including respiratory and central nervous system depression, decreased cardiac output, and hypotension. Approximately one-third of patients experience nausea, and morphine can increase the risk of aspiration, especially when continuous positive airway pressure (CPAP) is needed, due to its suppression of the respiratory center. Furthermore, its use in acute pulmonary edema has been linked to a higher incidence of mechanical ventilation, intensive care unit admissions, and mortality.
In the absence of high-quality data from randomized trials, current evidence suggests that morphine may cause harm in this context. As a result, it is no longer recommended for routine use in acute pulmonary edema.
However, administration of morphine may be justified in patients with persistent, intense chest pain that is resistant to nitrates. In such cases, low doses of morphine (1–2.5 mg) may help facilitate the tolerability of invasive ventilation; close monitoring for sedation is essential.
Ventilation Support
The first step in improving ventilation for patients with acute pulmonary edema is to ensure they are in a sitting position, which helps reduce the ventilation-perfusion mismatch.
Oxygen Therapy:
Oxygen is not recommended for routine use in patients without hypoxemia because hyperoxemia can lead to vasoconstriction, decreased cardiac output, and increased short-term mortality. Administering oxygen to a patient who is asphyxiating without hypoxemia may mask clinical deterioration and delay necessary treatment. Supplemental oxygen and assisted ventilation should only be used if oxygen saturation falls below 92%.
When necessary, oxygen should be administered to achieve a target oxygen saturation of 92–96% (with a guideline of 94–98% from the Ministry of Health of Ukraine). Depending on the clinical scenario, oxygen titration can be performed using various delivery devices, including:
- Up to 4 L/min via nasal cannulas
- 5–10 L/min via a face mask
- 15 L/min via a non-rebreather mask
- High-flow nasal cannulas with a fraction of inspired oxygen greater than 35%
For patients with chronic obstructive pulmonary disease (COPD), the target oxygen saturation is 88–92%, and a Venturi mask with inspired oxygen set at 28% is recommended.
Noninvasive Ventilation:
If the patient experiences respiratory distress, acidosis, or hypoxia despite supplemental oxygen, noninvasive ventilation is indicated. There is no significant clinical advantage of bi-level positive airway pressure (BiPAP) over continuous positive airway pressure (CPAP), so the choice of ventilation mode may depend on the specific characteristics of the care center and local availability. Noninvasive ventilation should be initiated with 100% oxygen, with recommended initial settings of 10 cm H2O for CPAP and 10/4 cm H2O (positive inspiratory pressure/expiratory positive airway pressure) for BiPAP. Contraindications to noninvasive ventilation include hypotension, potential pneumothorax, vomiting, and altered levels of consciousness.
Intubation:
If persistent hypercapnia, hypoxemia, or acidosis occurs despite noninvasive ventilation, intubation should be considered. Other indications for intubation include signs of physical exhaustion, decreased level of consciousness, or cardiogenic shock. Endotracheal intubation is indicated only in a limited number of cases and carries significant risks and complications. After intubation, continuous suctioning is often required, and ventilation may be challenging. Additionally, positive pressure ventilation can exacerbate hypotension.
Clinical case simulator “An interrupted symphony”
Medical training. A 74-year-old patient was brought to the hospital by the medical team, presenting…
Clinical case simulator “Mysteries of the heart”
Medical training. A 51-year-old female patient was brought by an emergency medical team to a…
From diagnosis to remission
A 34-year-old male patient was admitted to a hospital department presenting with symptoms of general…
A case of treatment of a patient with blood test abnormalities and fever
A 52-year-old man was admitted to the hematological center with a suspicion of a hematological…
A patient with severe neurological symptoms in the hematology department
A 69-year-old woman was hospitalized to the hematology department of the hospital with complaints of…
Choosing a treatment strategy for a patient with abnormalities in complete blood count
A 46-year-old woman was referred to a hematologist by her family doctor. The patient complains…
From chest pain to diagnosis in a 61-year-old patient
A 61-year-old woman consulted a hematologist with complaints of chest pain, weight loss, and general…
Objective structured clinical examination (OSCE)
Objective Structured Clinical Examination (OSCE) is a modern type of knowledge assessment used in medicine….
Cardiac pain and ECG changes. What can be detected from an ECG?
A 53-year-old man with a past medical history of diabetes and hypertension presents to the…
Unconsciousness and ECG changes in a patient with comorbidities
The patient was admitted to the cardiology department, where he received an appropriate treatment. After…
Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in a young woman
Case simulator Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in…
Pregnancy after myocardial revascularization
Clinical case simulator “Pregnancy after myocardial revascularization”. A young woman who has had multiple recurrent…
Chronic Myeloid Leukemia and Jaundice
A patient diagnosed with chronic myeloid leukemia suddenly develops jaundice. Is this a manifestation of…
Back pain in a woman
Simulator of a clinical case “Back pain in a woman”: the patient cries, having learned…
A Lady with a sudden cardiac pain
A sudden cardiac pain: what could have happened to Miss Laura Smith? What are the…
The rehabilitation program in patients with acute myocardial infarction
This scenario is a simulation of the clinical situation “The rehabilitation program in patients with…
Assessment the degree of ST segment elevation on the ECG, J-point
Do you know how to assess the degree of ST segment elevation on an ECG?…
Inotropes
Intravenous inotropic drugs are indicated for acute pulmonary edema when the patient exhibits hypotension, leading to reduced organ perfusion. Their use is limited to this clinical situation in critically ill patients, as they are associated with longer hospital stays and increased mortality. In cases of left ventricular dysfunction accompanied by hypotension, the first-line therapy is the intravenous infusion of dobutamine.
It is important to note that, in addition to its positive inotropic effects, dobutamine has peripheral vasodilator properties, which can exacerbate hypotension and may necessitate treatment with vasopressors. Additionally, dobutamine can induce arrhythmias and is contraindicated in patients with ventricular arrhythmias or tachysystolic forms of atrial fibrillation.
Another inotrope, milrinone, can also increase cardiac output and improve peripheral perfusion. However, it should be reserved for the short-term treatment of severe heart failure that has not responded to other therapies. Caution is advised with milrinone, as it may increase mortality in acute exacerbations of chronic heart failure.
Inotropes and vasopressors are critical in the management of acute heart failure.
| Drug | Bolus | Infusion |
|---|---|---|
| Dobutamine | No | 2-20 mcg/kg/min (beta+) |
| Dopamine | No | 3-5 mcg/kg/min (beta+) >5 mcg/kg/min (beta+, alpha+) |
| Milrinone | 25-75 mcg/kg for 10-20 minutes | 0.375-0.75 mcg/kg/min |
| Levosimendan | 12 mcg/kg for 10 minutes | 0.1 μg/kg/min (can decrease to 0.05 or increase to 0.2 μg/kg/min) |
| Norepinephrine | No | 0.2-1.0 mcg/kg/min |
| Epinephrine | 1 mg IV during resuscitation measures<br/> Repetition in 3-5 minutes | 0.05-0.5 mcg/kg/min |
Follow-up
Once the patient’s condition is stabilized, the underlying cause of acute pulmonary edema should be identified and treated. This includes reviewing the patient’s medications to determine if any, such as nonsteroidal anti-inflammatory drugs, verapamil, or diltiazem, may have contributed to the condition. Careful additional monitoring is also recommended, including daily weight monitoring, measurement of serum electrolytes, and assessment of renal function.
After stabilizing a patient with acute cardiogenic pulmonary edema, the goal of therapy is to improve long-term outcomes. If a preserved left ventricular ejection fraction is detected during echocardiography, primary attention should be paid to treating any concomitant diseases. This includes:
- Treating hypertension with antihypertensive drugs.
- Reducing pulmonary congestion and peripheral edema with diuretics.
- Controlling heart rate in cases of atrial fibrillation.
If there is evidence of reduced ejection fraction and chronic heart failure, ACE inhibitors, beta-blocker titration, and the use of drugs affecting mineralocorticoid receptors should be considered.
It is advisable to start ACE inhibitors 24-48 hours after the patient’s condition stabilizes, provided the patient is hemodynamically stable. Caution should be exercised when using ACE inhibitors in patients with hypotension or renal insufficiency, with close monitoring of blood pressure and renal function. Beta-blockers should be titrated from low doses as soon as the patient reaches a euvolemic state before discharge from the hospital. Mineralocorticoid receptor antagonists, such as spironolactone, are best initiated soon after discharge, with close monitoring of blood pressure, serum potassium, and renal function.
Recommendations for the Patient
- Lifestyle Changes:
- Smoking: Complete cessation.
- Diet: Follow cardiological recommendations, limiting salt intake.
- Fluid Restriction: Maximum of 2 liters per day (1.5 liters per day with pronounced CHF).
- Alcohol: No more than one unit per day.
- Physical Activity: Individualized rehabilitation program.
- Diagnostics:
- Echocardiography: Mandatory for all patients after acute pulmonary edema.
- Basic Cardiological Studies: ECG, lipid profile, glucose assessment, renal function assessment, including calculation of GFR.
- Other Tests: Liver function, thyroid function, iron content, and clinical blood analysis.
- Monitoring:
- Self-monitoring of symptoms, weight, and blood pressure.
- Regular examinations by a general practitioner (frequency determined by the severity and manifestations of CHF):
- Monitor symptoms, weight, blood pressure, and cardiorespiratory status.
- Manage risk factors and concomitant diseases (especially coronary heart disease, diabetes, COPD, impaired kidney function, sleep apnea, obesity, depression, osteoarthritis).
- Assess mental state and control available medications (which can be used as emergency aid in case of recurrent acute pulmonary edema).
- Monitor pathology (urea, creatinine, electrolytes, and clinical blood analysis).
- Medications that Improve Prognosis and Symptoms:
- ACE Inhibitors: Angiotensin II receptor blockers can be used in patients with CHF who are intolerant to ACE inhibitors.
- Beta-blockers: Indicated for patients with systolic heart failure; COPD is not a contraindication for prescribing beta-blockers (e.g., bisoprolol, carvedilol, metoprolol, nebivolol).
- Furosemide: For symptoms of fluid overload.
- Spironolactone: To be added if symptom control is insufficient.
- Digoxin: Considered for patients with concomitant atrial fibrillation or as an adjunct therapy for severe CHF inadequately controlled by the aforementioned drugs.
- Medications to Use with Caution:
- Contraindicated: Verapamil and diltiazem, NSAIDs or cyclooxygenase-2 inhibitors, corticosteroids.
- Vaccinations: Influenza, pneumococcus, COVID-19.
- Device Therapy for Patients with Moderate to Severe CHF: (To be assessed and recommended by a cardiologist if appropriate):
- Cardiac resynchronization therapy (e.g., if QRS is greater than 120 ms).
- Implanted cardioverter-defibrillator.
Conclusion
Clinical guidelines emphasize the lack of evidence supporting currently available treatments. There are also concerns about the effectiveness and safety of these treatments. Therefore, in recent years, there has been a shift toward favoring nitrates and noninvasive ventilation as first-line treatments. However, opioids and diuretics may still play a positive role in some patients.
References:
- 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) https://academic.oup.com/eurheartj/article/37/27/2129/1748921
- Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal, Volume 37, Issue 27, 14 July 2016, Pages 2129–2200, https://doi.org/10.1093/eurheartj/ehw128
- Purvey M, Allen G. Managing acute pulmonary oedema. Aust Prescr. 2017;40(2):59-63. doi:10.18773/austprescr.2017.012 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5408000/
- Acute cardiogenic pulmonary oedema. In: eTG complete [Internet]. Melbourne: Therapeutic Guidelines Limited; 2016. www.tg.org.au
- Coons JC, McGraw M, Murali S. Pharmacotherapy for acute heart failure syndromes. Am J Health Syst Pharm 2011;68:21-35. 10.2146/ajhp100202 [PubMed]
- Andrew Baird. Acute pulmonary oedemaю. Management in general practice. Australian Family Physician Vol. 39, No. 12, 2010: 910-914.
Clinical case simulator “An interrupted symphony”
Medical training. A 74-year-old patient was brought to the hospital by the medical team, presenting…
Clinical case simulator “Mysteries of the heart”
Medical training. A 51-year-old female patient was brought by an emergency medical team to a…
From diagnosis to remission
A 34-year-old male patient was admitted to a hospital department presenting with symptoms of general…
A case of treatment of a patient with blood test abnormalities and fever
A 52-year-old man was admitted to the hematological center with a suspicion of a hematological…
A patient with severe neurological symptoms in the hematology department
A 69-year-old woman was hospitalized to the hematology department of the hospital with complaints of…
Choosing a treatment strategy for a patient with abnormalities in complete blood count
A 46-year-old woman was referred to a hematologist by her family doctor. The patient complains…
From chest pain to diagnosis in a 61-year-old patient
A 61-year-old woman consulted a hematologist with complaints of chest pain, weight loss, and general…
Objective structured clinical examination (OSCE)
Objective Structured Clinical Examination (OSCE) is a modern type of knowledge assessment used in medicine….
Cardiac pain and ECG changes. What can be detected from an ECG?
A 53-year-old man with a past medical history of diabetes and hypertension presents to the…
Unconsciousness and ECG changes in a patient with comorbidities
The patient was admitted to the cardiology department, where he received an appropriate treatment. After…
Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in a young woman
Case simulator Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in…
Pregnancy after myocardial revascularization
Clinical case simulator “Pregnancy after myocardial revascularization”. A young woman who has had multiple recurrent…
Chronic Myeloid Leukemia and Jaundice
A patient diagnosed with chronic myeloid leukemia suddenly develops jaundice. Is this a manifestation of…
Back pain in a woman
Simulator of a clinical case “Back pain in a woman”: the patient cries, having learned…
A Lady with a sudden cardiac pain
A sudden cardiac pain: what could have happened to Miss Laura Smith? What are the…
The rehabilitation program in patients with acute myocardial infarction
This scenario is a simulation of the clinical situation “The rehabilitation program in patients with…
Assessment the degree of ST segment elevation on the ECG, J-point
Do you know how to assess the degree of ST segment elevation on an ECG?…
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Сounseling a patient with suspected Takotsubo-syndrome OSCE guides
The onset of the consultation Wash hands and put on PPE if necessary. Introduce yourself…
Takotsubo syndrome
Takotsubo syndrome is a condition characterized by the sudden onset of acute, transient (lasting up…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…
Symptomatic bradycardia
Symptomatic bradycardia occurs when the heart rate drops below 50 beats per minute. Most often,…
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
SAVED VTE Score
SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…