Counseling a patient who is taking warfarin / OSCE guide

Before initiating anticoagulation therapy with warfarin
Before initiating anticoagulation therapy an assessment of the patient’s coagulation status is necessary, including:
- a baseline INR
- indication for treatment
- apropriate INR target range
- proposed duration of treatment
All these results should be recorded in the patient’s case records and oral anticoagulation therapy booklet.
Before Counselling
Before Counselling physician should review the patient’s medical background to establish the current indication for warfarin and the patient’s target INR range.
Before adjusting the dose during maintaining treatment
Before adjusting the dose of warfarin the physician should review:
- the previous doses warfarin
- earlier INR results
- any changes in the patient’s clinical condition
- any changes in medication
- any changes in lifestyle
- alcohol consumption
Target INR ranges
The most common target INR is 2.5. Others are:
| Recurrent VTE (DVT or PE) despite adequate anticoagulation | 3.5 |
| Cardioversion | Pre – 3.0 Post – 2.5* |
| Mechanical Heart Valves | See below |
*The 2016 European Society of Cardiology (ESC) guidelines on cardioversion state that patients who have been in AF for longer than 48 hours should start OAC therapy at least 3 weeks before cardioversion and continue for 4 weeks afterwards (in those without a need for long-term anticoagulation).
Atrial fibrillation Anticoagulation is normally offered to patients with a CHADSVASc score ≥ 2 and considered in men with a CHADSVASc score of 1.
Warfarin is not usually indicated for ischaemic stroke without atrial fibrillation (except in antiphospholipid syndrome), retinal vessel occlusion, peripheral artery thrombosis, coronary artery graft or coronary angioplasty, and stents.
Cardioversion
Anticoagulation for 4 weeks before and for 3 months afterward. To minimize cardioversion cancellations due to low INRs on the day of the procedure we recommend a target INR of 3.0 prior to the procedure and 2.5 afterward (Oxford guidelines).
*The 2016 European Society of Cardiology (ESC) guidelines on cardioversion state that patients who have been in AF for longer than 48 hours should start OAC therapy at least 3 weeks before cardioversion and continue for 4 weeks afterwards (in those without a need for long-term anticoagulation).
Mechanical Heart Valves. Target INR range based on indications
| Target INR in mechanical heart valve replacement Mechanical Prosthesis thrombogenicity* | Isolated Aortic Valve Replacement | Mitral or Tricuspid Valve Replacement, or |
| No risk factors** | AVR with Risk factors ** | |
| Low (most current valves) | 2.5 | 3.0 |
| Medium | 3.0 | 3.5 |
| High | 3.5 | 3.5*** |
*Prosthesis thrombogenicity:
- Low: Carbomedics (aortic position), Medtronic Hall, St Jude Medical (without silzone)
- Medium: Bjork-Shiley, other bileaflet valves
- High: Starr-Edwards, Omniscience, Lillehei-Kaster.
**Patient-related risk factors for thrombosis:
- Mitral, tricuspid or pulmonary position
- Previous arterial thromboembolism
- Atrial fibrillation
- Left atrium diameter >50 mm
- Mitral stenosis of any degree
- Left ventricular ejection fraction< 35%.
***Was 4.0 in ESC guideline
Counseling steps:
- Opening the consultation
- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role
- Confirm the patient’s name and date of birth
- Explain the reason for the consultation
- Ideas, concerns and expectations
- Explore what the patient currently understands about warfarin and why they are being prescribed it
- Ask if the patient has any concerns about warfarin
- Explore what the patient is hoping to get out of the consultation
- How warfarin works
- Explain that warfarin works by thinning the blood
- Explain what warfarin can be used to treat
- Explain that the action of warfarin can be reversed with an antidote if needed
- INR
- Explain what INR is
- Explain what the patient’s target INR range is
- Explain how INR is monitored
- How to take warfarin
- Explain that warfarin should be taken at the same time each day
- Explain the different types of warfarin tablets
- Explain what the patient should do if they forget a dose
- Advise the patient to let medical professionals know that they take warfarin when they are being prescribed new medications
- Advise the patient to let the team managing their anticoagulation know when they start taking a new medication
- Advise the patient about the importance of effective contraception if taking warfarin (if relevant)
- Bleeding whilst taking warfarin
- Explain that the main side effect of warfarin is bleeding more easily than normal
- Explain the common types of ‘less serious bleeding’ and what to do if they experience them
- Explain the rarer types of ‘serious bleeding’ and what to do if they experience them
- Other side effects of warfarin
- Explain the common side effects of warfarin (other than bleeding)
- Explain the rarer and more serious side effects of warfarin
- Lifestyle advice
- Advise the patient about the impact of diet on the effect of warfarin
- Advise the patient about the impact of alcohol on the effect of warfarin
- Advise the patient about brushing teeth, shaving and dental procedures
- Yellow booklets and alert card
- Provide the patient with information about the INR monitoring booklet and patient information booklet
- Explain the importance of carrying the anticoagulant alert card with them at all times
- Closing the consultation
- Summarise the key points back to the patient
- Ask the patient if they have any questions or concerns that have not been addressed
- Arrange appropriate follow-up
- Thank the patient for their time
- Dispose of PPE appropriately and wash your hands
- Key communication skills
- Active listening
- Summarising
- Signposting
Join our Simulation Training to gain clinical experience
Clinical case simulator “An interrupted symphony”
Medical training. A 74-year-old patient was brought to the hospital by the medical team, presenting…
Clinical case simulator “Mysteries of the heart”
Medical training. A 51-year-old female patient was brought by an emergency medical team to a…
From diagnosis to remission
A 34-year-old male patient was admitted to a hospital department presenting with symptoms of general…
A case of treatment of a patient with blood test abnormalities and fever
A 52-year-old man was admitted to the hematological center with a suspicion of a hematological…
A patient with severe neurological symptoms in the hematology department
A 69-year-old woman was hospitalized to the hematology department of the hospital with complaints of…
Choosing a treatment strategy for a patient with abnormalities in complete blood count
A 46-year-old woman was referred to a hematologist by her family doctor. The patient complains…
From chest pain to diagnosis in a 61-year-old patient
A 61-year-old woman consulted a hematologist with complaints of chest pain, weight loss, and general…
Objective structured clinical examination (OSCE)
Objective Structured Clinical Examination (OSCE) is a modern type of knowledge assessment used in medicine….
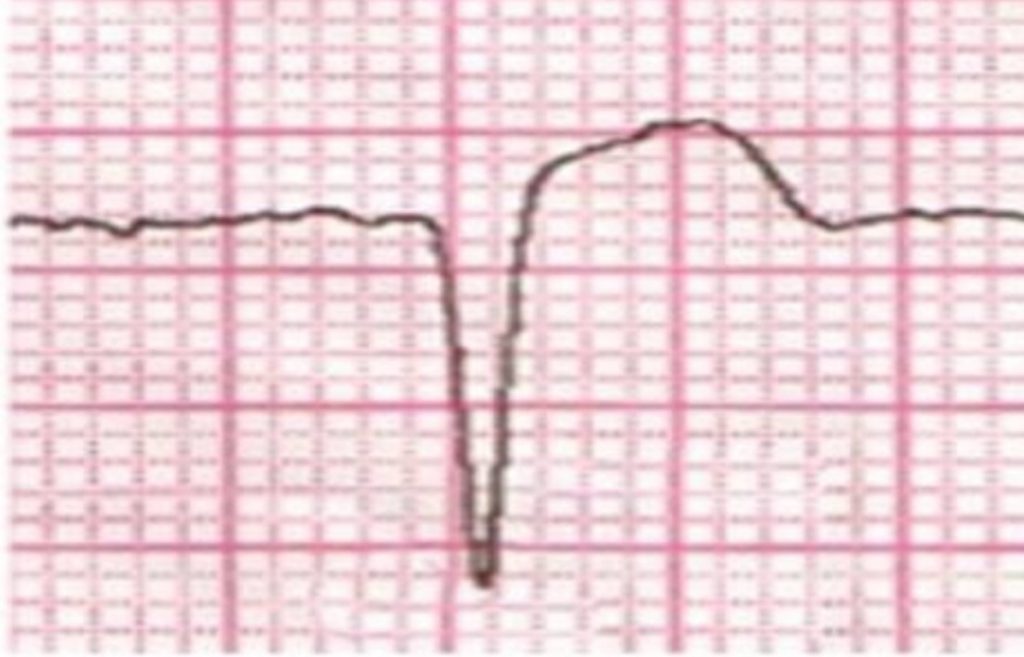
Cardiac pain and ECG changes. What can be detected from an ECG?
A 53-year-old man with a past medical history of diabetes and hypertension presents to the…
Unconsciousness and ECG changes in a patient with comorbidities
The patient was admitted to the cardiology department, where he received an appropriate treatment. After…
Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in a young woman
Case simulator Choice of dual antiplatelet therapy (DAPT) duration after stenting of coronary arteries in…
Pregnancy after myocardial revascularization
Clinical case simulator “Pregnancy after myocardial revascularization”. A young woman who has had multiple recurrent…
Chronic Myeloid Leukemia and Jaundice
A patient diagnosed with chronic myeloid leukemia suddenly develops jaundice. Is this a manifestation of…
Back pain in a woman
Simulator of a clinical case “Back pain in a woman”: the patient cries, having learned…
A Lady with a sudden cardiac pain
A sudden cardiac pain: what could have happened to Miss Laura Smith? What are the…
The rehabilitation program in patients with acute myocardial infarction
This scenario is a simulation of the clinical situation “The rehabilitation program in patients with…
Assessment the degree of ST segment elevation on the ECG, J-point
Do you know how to assess the degree of ST segment elevation on an ECG?…
Opening the consultation
- Wash your hands and don PPE if appropriate.
- Introduce yourself to the patient including your name and role.
- Confirm the patient’s name and date of birth.
- Explain the reason for the consultation
Ideas, concerns and expectations
- Explore what the patient currently understands about warfarin and why they are being prescribed it
- Ask if the patient has any concerns about warfarin
- Explore what the patient is hoping to get out of the consultation
| Ideas | Explore what the patient currently understands about warfarin and why they are being prescribed it | “Have you heard of warfarin?” “What do you already know about warfarin?” “Do you know why people take warfarin?” |
| Concerns | Ask if the patient has any concerns about warfarin | “Is there anything that worries you about taking warfarin?” |
| Expectations | Explore what the patient is hoping to get out of the consultation | “What were you hoping we’d discuss today?” |
How warfarin works
- Explain that warfarin works by thinning the blood
- Explain what warfarin can be used to treat
- Explain that the action of warfarin can be reversed with an antidote if needed
Using patient-friendly language, explain how warfarin works.
“Warfarin is a medication that helps “thin” your blood to decrease your body’s chance of forming harmful clots. Unwanted blood clots may cause strokes, heart attacks, or other potentially harmful events such as clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism).”
“Warfarin is a type of medicine known as an anticoagulant. It helps to thin the blood, making it less likely that a dangerous blood clot could form.”
“Warfarin can be used to treat people who have a previous blood clot in the leg or lungs. It can also be used to prevent future blood clots in people who are at high risk of having them in the future, such as people with an irregular heartbeat or an artificial heart valve.”
“There are proteins in your blood to help form clots. These proteins are made by your liver with the help of vitamin K. Warfarin works by blocking the effects of vitamin K, making it harder for your body to form clots. In order to make sure the amount of warfarin you’re taking is right for you, your healthcare professional will test your blood periodically.”
“The action of warfarin can be rapidly reversed with an antidote in situations where we need to reduce the risk of bleeding.”
“Following the administration of warfarin an observable anticoagulation effect is delayed. The delay may range from two to seven days because warfarin does not act directly on the inactive clotting factors already in circulation but on the rate of synthesis of new factors by the liver. “
INR
- Explain what INR is
- Explain what the patient’s target INR range is
- Explain how INR is monitored
Explain the role of INR in monitoring the effect of warfarin.
“The INR is a measure of how long it takes blood to clot. In healthy people an INR of 1 is normal. Since you are at a higher risk for blood clots we want your blood to be thinner than normal and therefore take longer to clot. As a result, the target range for your INR would be between 2-3, meaning it takes two to three times as long for your blood to clot compared to someone not taking warfarin.”
“In order to ensure that we keep your blood within the necessary range we will need to monitor your INR level every so often; this is done through a blood test. The blood tests will initially be frequent (every 3-4 days until two consecutive readings are within range), and then after this, you will be tested twice weekly for 1-2 weeks (again until two consecutive readings within range). Thereafter, testing can increase to longer periods (e.g. every 12 weeks). Your dose of warfarin will be adjusted based on the INR results with the aim of keeping it within the target range.”
Frequency of monitoring
During the induction and initial stabilization of patients on warfarin, daily INR measurements are often necessary, particularly with the more aggressive induction regimens. After initial stabilization the INR will, in most cases, dictate the frequency of monitoring.
Weekly monitoring is advised for four to six weeks after stabilization, gradually changing to every one to two months if concordance and control are good.
“It is very important to have your blood tests regularly (preferably in a warfarin clinic)”.
How to take warfarin
- Explain that warfarin should be taken at the same time each day
- Explain the different types of warfarin tabletsExplain what the patient should do if they forget a dose
- Advise the patient to let medical professionals know that they take warfarin when they are being prescribed new medications
- Advise the patient to let the team managing their anticoagulation know when they start taking a new medication
- Advise the patient about the importance of effective contraception if taking warfarin (if relevant)
Key points to communicate when discussing warfarin use:
- “Warfarin should be taken at the same time each day to keep the levels of warfarin steady.”
- “Tablets have different colours depending on their strength (e.g. 0.5mg white; 1mg brown; 3mg blue; 5mg pink).”
- “If you forget to take a dose you should take it as soon as you remember, but if you don’t remember till the following day you should skip the missed dose. You should never take two doses together to make up for a missed dose and you should inform your doctor or warfarin clinic about any missed doses at your next appointment.”
- “Whenever you are going to purchase or be prescribed a new medication you should let the doctor or pharmacist know that you take warfarin so they can avoid prescribing medications which alter your warfarin level.”
- “When you start taking a new medication you should let your doctor or anticoagulant clinic know so that they can consider if your warfarin levels need monitoring more frequently.”
- “You should continue to take your warfarin tablets regularly until you have been told to stop.”
- “Warfarin is not safe to be used during pregnancy and therefore you should have an effective contraceptive method in place before you start taking warfarin.”
- “You must inform anticoagulant healthcare staff if you think you have taken too much warfarin or have missed any doses.”
- “You must inform the relevant healthcare professionals if you start, stop or change the dose of your medicines, or if your diet changes substantially (eg. intake of broccoli, lettuce or spinach /)”Other medicines” include not only prescribed drugs but also products that may be brought without prescription, such as aspirin, and medicines containing aspirin, vitamins, food supplements and herbal or homoeopathic remedies.”
- “If you require surgery, dental work, or any other invasive procedure you may need stop taking warfarin temporarily. You should discuss your warfarin management with a healthcare professional prior to the procedure”.
Selected examples of drug interactions with warfarin:
| Drugs that enhance the anticoagulant effect | Drugs that reduce the anticoagulant effect |
| Allopurinol Amiodarone Aspirin Azole antifungals (fluconazole, itraconazole, ketconazole, miconazole) Cimetidine Ciprofloxacin Entacapone Fibrates Fluvastatin Metronidazole Omeprazole Simvastatin Tamoxifen Testosterone Tetracyclines Thyroxine Tramadol SSRIs | Carbamazepine Oestrogens Phenytoin* Primidone Progestogens Rifamycins Vitamin K present in some enteral feeds |
* The metabolism of coumarins is accelerated by phenytoin (there is a possibility of a reduced anticoagulant effect, but enhancement has also been reported).
Erythromycin and other macrolides interact with warfarin unpredictably and only affect certain individuals.
Surgery and warfarin therapy
When a patient who is receiving long-term warfarin therapy requires surgery a variety of approaches may be considered.
- If the risk f subsequent thromboembolism is low it may be acceptable to discontinue the warfarin in advance of the procedure.
- For patients with a greater risk, the dose may be lowered and the operation performed when the INR is at an acceptable level (ie., below 2.5).
- A third alternative is to reduce the anticoagulant effect with vitamin K just prior to the surgery and operate under prophylactic cover of heparin, with the aim of reintroducing in the immediate post-operative period.
Dental advice
Many dentists appear to be unaware of the specific needs of the patients who are receiving anticoagulants and perform procedures from dental hygiene to multiple extractions without managing the treatment or referring to others.
Minor dental surgical procedures can be carried out safely as long as the patient’s INR is below 4.0. Examples of the procedures likely to be carried out in primary care would be the simple extraction of up to the three teeth, crown work, and cosmetic dentistry. An INR measurement should be taken within 72 hours of the procedure.
Pharmaceutical advice for patients on the management of clots in the post-operative dental period:
The physician should advise the patient to:
- rest while the local anesthetic wears off and the clot fully forms (this usually takes two to three hours)
- take paracetamol if pain control is needed (NSAIDs and aspirin or products containing these medicines should be avoided)
- avoid rinsing the mouth for 24 hours unless specifically advised to do so by a healthcare professional
- avoid sucking hard or disturbing the clot with the tongue or anything else
- avoid hot liquids and hard foods for the rest of the day
- avoid chewing on the affected side until they are sure that a stable clot has formed
- rinse the mouth with warm salty water three or four times the day after treatment
If the bleeding continues or restarts you should advise the patient to apply pressure over the bleeding area using a clean, damp folded handkerchief or gauze pad. The pad should be placed over the site of the bleeding and the patient should bite down firmly for 20 minutes while sitting quietly in a chair.
Bleeding whilst on warfarin
- Explain that the main side effect of warfarin is bleeding more easily than normal
- Explain the common types of ‘less serious bleeding’ and what to do if they experience them
- Explain the rarer types of ‘serious bleeding’ and what to do if they experience them
The main side effect of warfarin involves bleeding more easily than normal (e.g. epistaxis, bleeding gums, heavier periods, bruising). These side effects most commonly occur in the first few weeks of treatment or when the patient is unwell. It is important to discuss the different types of bleeding the patient may experience and inform them what to do in these situations.
| Less serious bleeding Minor bleeding | Serious bleeding Major bleeding |
| “It is normal to bleed more easily when taking warfarin as the medication works by thinning the blood. Common types of bleeding include – periods that are heavier and last longer than normal – bleeding for a little longer than usual if you cut yourself – occasional nosebleeds (that last for less than 10 minutes) – bleeding from your gums when you brush your teeth – bruised that come up more easily and take longer to fade than usual. This type of bleeding is not dangerous and should stop by itself. If it happens, keep taking the warfarin, but tell your doctor if the bleeding bothers you or does not stop.” | “Occasionally, you can have serious bleeding from taking warfarin. This can be dangerous and needs urgent medical attention.” “Stop taking warfarin and call your doctor or anticoagulant clinic, or go to A&E if you experience: – red pee or black poo, – large bruises or bruises that happen for no reason, – nosebleeds that last longer than 10 minutes, – blood in your vomit or you’re coughing up blood, – severe headaches, fits (seizures), changes to your eyesight, numbness or tingling in your arms or legs, or feeling very tired, weak, or sick – these can be signs of bleeding in your brain – any bleeding from a cut or injury that will not stop or slow down” |
Other side effects of warfarin
- Explain the common side effects of warfarin (other than bleeding)
- Explain the rarer and more serious side effects of warfarin
| Common side effects | Serious side effects |
| Common side effects (other than bleeding) of warfarin include: – a mild rash – hair loss These side effects are typically mild and the patient should be advised to contact their doctor or pharmacist if they become bothersome. | Serious side effects of warfarin can include: – jaundice – skin necrosis As a result, patients should be advised to seek urgent medical review if they develop: – yellowing of the skin – painful swollen areas of skin |
Lifestyle advice
- Advise the patient about the impact of diet on the effect of warfarin
- Advise the patient about the impact of alcohol on the effect of warfarin
- Advise the patient about brushing teeth, shaving and dental procedures
| Diet | Drastic changes in diet, especially an increase in consumption of foods high in vitamin K (such as broccoli, kale, or spinach) can potentially affect the control of anticoagulation. If the patient ever wishes to significantly change their diet, they should inform the anticoagulant clinic so necessary dose adjustments and monitoring requirements can be fulfilled. “Since vitamin K and warfarin work against each other, the amount of vitamin K in your diet can change warfarin’s effects. It is important to keep your dietary intake of vitamin K consistent. Foods such as green leafy vegetables and certain oils have higher contents of vitamin K. (See the table below for a chart of vitamin K content in selected foods). If you DECREASE your intake of vitamin K (eat fewer foods containing vitamin K) your dose of warfarin may need to be lowered to prevent bleeding. If you INCREASE your intake of vitamin K, your dose of warfarin may need to be increased to prevent blood clots. A MAJOR change in your vitamin K intake can affect your PT/INR, but normal daily variation in the foods you eat is okay. You DON’T have to avoid foods that are high in vitamin K, just keep your diet consistent. You should let your healthcare professional know if there is going to be a major change in your diet, so your PT/INR can be closely monitored” Many people are on special diets, such as the Atkin’s or South Beach diets, to lose weight. These diets are high-protein diets and can also affect the way warfarin works in your body. Once you take a dose of warfarin, some of it binds to protein in your bloodstream. While warfarin is attached to this protein, it has no effect on your body. It’s thought that high protein diets can increase the number of proteins in your body and cause more warfarin to be bound to protein. This causes a DECREASE in warfarin available to prevent clots, so your warfarin dose may need to be increased. Always check with your healthcare professional before starting any special diets, so your PT/INR can be closely monitored. Certain foods can also affect how your liver clears warfarin from your body, causing warfarin levels to increase or decrease. Examples include alcohol, cranberry products (e.g., juice, supplements), and possibly grapefruit or grapefruit juice. Too much alcohol, cranberry products, or grapefruit products can INCREASE warfarin’s effect and increase your risk of bleeding. Avoid or limit your intake of alcohol, cranberry products, and grapefruit or grapefruit juice. Make sure your healthcare professional knows if your diet contains any of these products, so your PT/INR can be closely monitored. Cranberry juice is also known to interact with warfarin and enhance its anticoagulant effect and therefore it should be avoided. “People on vitamin K-rich diets should not change eating habits without at the same time reducing the warfarin dosage, because excessive anticoagulation and bleeding may occur.” |
| Alcohol | Patients should limit their alcohol intake to a maximum of one or two drinks a day and never binge drink. If there are major changes in alcohol consumption (e.g. the patient stops drinking, or starts drinking more) the INR can be affected. “People should limit the amount of alcohol to a maximum of one or two drinks a day and never bridge drink.” |
| Other | Patients should be advised to take extra care when carrying out routine tasks such as brushing teeth or shaving; a soft toothbrush or an electric razor can help. Patients should also be advised to inform their dentist that they take warfarin when booking an appointment as this may have implications for dental procedures. “Other things to remember when taking warfarin In addition to foods, many prescription and over-the-counter drugs, including vitamins and herbal supplements, can affect your warfarin level. You should not start, stop, or change doses of any drugs or supplements without first talking with your healthcare professional. Try to keep a healthy, well-balanced diet and keep your vitamin K intake consistent. Take your warfarin dose around the same time each day. If you miss a dose, take it as soon as you remember. If it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Don’t double up doses without checking with your healthcare professional. Tell your healthcare professional immediately if you have unusual bleeding or bruising, black or bloody stools, blood in the urine, or stomach pain.” “People should avoid activities which could cause abrasion, bruising or cuts (eg., contact sports, gardening, sewing), or at least use protection.” People should avoid insect bites, especially on their legs, and should use a repellent when exposed to insects. Patients with deep vein thrombosis should be given the following additional lifestyle advice: regular walking exercise helps to reduce the risk of further deep vein thrombosis and improves circulation in the affected limb the affected leg should be elevated when sitting “If you are traveling for any length of time will need to move your dosing time gradually – say by an hour a day – to a time that is convenient to the new zone. You may also need to have an INR check while you are away.” |
Yellow booklets and alert card
- Provide the patient with information about the INR monitoring booklet and patient information booklet
- Explain the importance of carrying the anticoagulant alert card with them at all
At the start of treatment, all patients should be provided with two yellow anticoagulant booklets, an INR monitoring booklet, and a patient information booklet. Patients should also be provided with an anticoagulant alert card.
Patients should be advised to always carry the anticoagulant alert card with them in case of an emergency and always take the yellow INR monitoring book with them to each appointment at the anticoagulant clinic and if possible to other appointments (e.g. GP, pharmacy reviews, dental appointments, etc).
The patient information book is a useful resource since it provides the patient with a point of reference and reinforces what has been covered in this guide.
Closing the consultation
- Summarise the key points back to the patient
- Ask the patient if they have any questions or concerns that have not been addressed
- Arrange appropriate follow-up
- Thank the patient for their time
- Dispose of PPE appropriately and wash your hands
Key communication skills
Summarise the key points back to the patient.
Ask the patient if they have any questions or concerns that have not been addressed.
If you feel that the patient would benefit from a recap session, arrange a follow-up appointment (face-to-face or telephone) and also direct the patient to the yellow anticoagulant information booklet for further reading.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Supplements materials
Vitamin K Content of Selected Foods
* Note: This is NOT a list of foods to avoid. This list provides information on the vitamin K content of certain foods.
| Foods | Low | Moderate | High |
| Vegetables | Green beans | Asparagus | Broccoli |
| Carrots | Avocado | Brussels sprouts | |
| Cauliflower | Red Cabbage | Cabbage | |
| Celery | Green peas | Collard greens | |
| Corn | Endive (raw) | ||
| Cucumber (peel removed) | Pickle (dill) | Kale (raw leaf) | |
| Eggplant | Lettuce (iceberg) | Lettuce (bib, red leaf) | |
| Mushrooms | Mustard greens (raw) | ||
| Onions | Parsley | ||
| Green pepper | Spinach | ||
| Potato | Turnip greens (raw) | ||
| Pumpkin | Watercress (raw) | ||
| Sauerkraut (canned) | Swiss chard | ||
| Tomato | |||
| Fruits | Apple | ||
| Banana | |||
| Blueberries | |||
| Grapes | |||
| Orange | |||
| Meats | Beef | ||
| Chicken | |||
| Pork | |||
| Tuna | |||
| Turkey | |||
| Fats and Oils | Corn oil | Margarine | Mayonnaise |
| Peanut oil | Olive oil | Canola oil | |
| Safflower oil | Soybean oil | ||
| Sesame oil | |||
| Sunflower oil | |||
| Dairy Products | Butter | ||
| Cheese (cheddar) | |||
| Eggs | |||
| Sour cream | |||
| Yogurt | |||
| Beverages | Coffee | ||
| Cola | |||
| Fruit juices | |||
| Milk | |||
| Tea (black) | Tea (green)** |
- Clotcare Online Resource at www.clotcare.com. (Accessed April 20, 2005).
** There is some controversy as to whether brewing green tea alters the vitamin K content and/or whether green tea may alter the effect of warfarin by some other mechanism.
Clinical case simulator “An interrupted symphony”
Medical training. A 74-year-old patient was brought to the hospital by the medical team, presenting…
Clinical case simulator “Mysteries of the heart”
Medical training. A 51-year-old female patient was brought by an emergency medical team to a…
From diagnosis to remission
A 34-year-old male patient was admitted to a hospital department presenting with symptoms of general…
A case of treatment of a patient with blood test abnormalities and fever
A 52-year-old man was admitted to the hematological center with a suspicion of a hematological…
A patient with severe neurological symptoms in the hematology department
A 69-year-old woman was hospitalized to the hematology department of the hospital with complaints of…
Choosing a treatment strategy for a patient with abnormalities in complete blood count
A 46-year-old woman was referred to a hematologist by her family doctor. The patient complains…
Potential Interactions of Dietary Supplements with Warfarina
| Potential Increase in Risk of Bleeding | ||
| Acetyl-L-carnitine | Fish oil | Mate |
| Arnica | Flaxseed, Flaxseed oil | Melatonin |
| Alcohol, acute use | Fo-ti | Mesoglycan |
| Bishop’s weed | Forskolin | Milk thistle |
| Black tea | Forsythia | N-acetyl glucosamine |
| Bladderwrack | Gamma-linolenic acid | Nattokinase |
| Boldo | Garlic | Oolong tea |
| Borage seed oil | Ginger | Pantethine |
| Burdock | Ginkgo | Papaya |
| Caffeine | Ginseng, Siberian | Peppermint oil |
| Chondroitin sulfate | Glucosamine | Propionyl-L-carnitine |
| Cod liver oil | Grapefruit, Grapefruit juice | Red clover |
| Coltsfoot | Guarana | Reishi mushroom |
| Cranberry, cranberry juice | Guggul | Resveratrol |
| Danshen | Holy basil | Saw palmetto |
| Devil’s claw | Honeysuckle | Sea buckthorn |
| Dong quai | Horse chestnut | Tiratricol |
| Epimedium | Ipriflavone | Turmeric |
| Eucalyptus oil | Jiaogulan | Vinpocetine |
| Evening primrose oil | Kava | Vitamin A |
| Fenugreek | L-carnitine | Vitamin E |
| Feverfew | Lycium | Willow bark |
| Wintergreen | ||
| Possible Decrease in Warfarin’s Effects | ||
| Acerola | ||
| Alcohol, chronic use | ||
| Alfalfa | ||
| Cherokee rosehip | ||
| Chlorella | ||
| Coenzyme Q10 | ||
| Corn silk | ||
| EDTA | ||
| Ginseng, American | ||
| Ginseng, Panax | ||
| Green tea | ||
| Limonene | ||
| Rose hip | ||
| Smartweed | ||
| Soy | ||
| Spinach | ||
| St. John’s wort | ||
| Stinging nettle | ||
| Vitamin C | ||
| Vitamin K | ||
| Watercress |
aAdapted from Natural Medicines Comprehensive Database at www.naturaldatabase.com. (Accessed 4/21/05).
Dialogue Simulator – Communication with a patient starting warfarin:
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
References:
- What You Should Know About Your Diet and Warfarin. PHARMACIST’S LETTER / Prescriber’s Letter to give to their patients. P.O. Box 8190, Stockton, CA 95208. May 2005 ~ Volume 21 ~ Number 210507, 8 p.
- Beatty SJ, Mehta BH, Rodis JL. Decreased warfarin effect after initiation of high-protein, lowcarbohydrate diets. Ann Pharmacother 2005;39:744
- Committee on Safety of Medicines (CSM). Current Problems in Pharmacovigilance 2003;29:8.
- Shields KM. Possible Cranberry and Warfarin Interaction. Pharmacist’s Letter/Prescriber’s Letter 2003;19(11):191103.
- Havrda DE, Mai T, Chonlahan J. Enhanced antithrombotic effect of warfarin associated with low-dose alcohol consumption. Pharmacotherapy 2005;25:303-7.
- OXFORD HAEMOPHILIA AND THROMBOSIS CENTRE PROTOCOLS FOR OUTPATIENT ORAL ANTICOAGULATION WITH VITAMIN K ANTAGONISTS. Prepared by D. Keeling with input and review from S. Shapiro, N. Curry, V. Price, and L. Mulholland.AC Protocols version 4.1 May 2017
- Paulus Kirchhof, Stefano Benussi, Dipak Kotecha, Anders Ahlsson, Dan Atar, Barbara Casadei, Manuel Castella, Hans-Christoph Diener, Hein Heidbuchel, Jeroen Hendriks, Gerhard Hindricks, Antonis S. Manolis, Jonas Oldgren, Bogdan Alexandru Popescu, Ulrich Schotten, Bart Van Putte, Panagiotis Vardas, Stefan Agewall, John Camm, Gonzalo Baron Esquivias, Werner Budts, Scipione Carerj, Filip Casselman, Antonio Coca, Raffaele De Caterina, Spiridon Deftereos, Dobromir Dobrev, José M. Ferro, Gerasimos Filippatos, Donna Fitzsimons, Bulent Gorenek, Maxine Guenoun, Stefan H. Hohnloser, Philippe Kolh, Gregory Y. H. Lip, Athanasios Manolis, John McMurray, Piotr Ponikowski, Raphael Rosenhek, Frank Ruschitzka, Irina Savelieva, Sanjay Sharma, Piotr Suwalski, Juan Luis Tamargo, Clare J. Taylor, Isabelle C. Van Gelder, Adriaan A. Voors, Stephan Windecker, Jose Luis Zamorano, Katja Zeppenfeld, 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS, EP Europace, Volume 18, Issue 11, November 2016, Pages 1609–1678, https://doi.org/10.1093/europace/euw295
Сounseling a patient with suspected Takotsubo-syndrome OSCE guides
The onset of the consultation Wash hands and put on PPE if necessary. Introduce yourself…
Counseling of a patient with symptomatic bradycardia – OSCE guide
https://clincasequest.hospital/course/interrupted-symphony/ The onset of the consultation Wash hands and put on PPE if necessary. Introduce…
Checklist – Counseling “Explain a bone marrow aspiration”
IntroductionPointsIntroduces and identifies patient1Gains consent1Explore Checks patients understanding for reason for Bone Marrow Aspiration2Check’s patients understanding…
Checklist – Counseling “History of Acute Intermittent Porphyria”
IntroductionPointsIntroduce and check the details1Consent1Presenting Compliant Elicit intermittent nature of abdominal pain1Details on length of suffering…
Calgary-Сambridge guide to the medical interview
This manual was developed by specialists from the Faculty of Medicine of the University of…
Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents /OSCE guide
Opening the consultation Wash your hands and don PPE if appropriate Introduce yourself to the…