Focused Assessment with Sonography for Trauma (FAST): Online Calculator

Focused Assessment with Sonography for Trauma (FAST) predicts the presence of pericardial or intra-abdominal injury after penetrating or blunt trauma.
- FAST should be used liberally in the evaluation of trauma patients.
- Especially useful in patients with penetrating thoracic trauma and in unstable patients after blunt abdominal trauma.
FAST is a rapid, non-invasive, and repeatable imaging modality that can guide the surgeon in the decision to operate.
Performed in trauma bay (does not require patient transport out of the emergency department, which is risky in unstable patients).
FAST results alone should not determine the decision to operate. However, FAST can be a helpful adjunct in clinical decision making, particularly in an unstable blunt trauma patient in order to rapidly assess the chest and abdomen for potential causes of hypotension.
Most clinicians use the low-frequency phased array ultrasound probe (a.k.a. cardiac probe), to obtain all windows in FAST.
| Pericardial fluid | Absent |
| Present | |
| Equivocal | |
| Right upper quadrant (Morison’s pouch) fluid | Absent |
| Present | |
| Equivocal | |
| Left upper quadrant (splenorenal recess) fluid | Absent |
| Present | |
| Equivocal | |
| Suprapubic fluid | Absent |
| Present | |
| Equivocal |
Most clinicians use the low-frequency phased array ultrasound probe (a.k.a. cardiac probe), to obtain all windows in FAST.
| Pericardial | place the probe in the subxiphoid area and orient it towards the patient’s left shoulder. Apply downward pressure to look under the costal margin and towards the heart. The heart and pericardium will come into view, allowing inspection for hemopericardium and ultrasound findings of cardiac tamponade. |
| Right upper quadrant | place probe in right anterior to the midaxillary line (between 11th–12th ribs). Visualization of the hepatorenal recess (Morison’s pouch) allows the assessment of hemoperitoneum in the right upper quadrant. Blood most likely accumulates here if hemoperitoneum is present. |
| Left upper quadrant | apply transducer firmly onto the skin in the left posterior axillary line (between the 9th–10th ribs) to visualize splenorenal and subphrenic spaces. In practice, it is important to remember that the right and left upper quadrant views are often more posterior than anticipated. It can be helpful to bring the probe all the way down to the stretcher in order to best visualize these windows. |
| Suprapubic | place transducer superior to pubic symphysis and fan probe inferiorly to visualize the bladder. |
Using bedside ultrasound, assess for fluid in each of the following areas:
| Fluid present? | |||
| Pericardial fluid | Absent | Present | Equivocal |
| Right upper quadrant (Morison’s pouch) fluid | Absent | Present | Equivocal |
| Left upper quadrant (splenorenal recess) fluid | Absent | Present | Equivocal |
| Suprapubic fluid | Absent | Present | Equivocal |
Management
Suggested management (clinician must consider additional clinical information including hemodynamic stability and clinical suspicion for injury):
| Pericardial FAST (penetrating thoracic trauma) | |
| Positive | emergent surgical intervention recommended. Median sternotomy preferred if the patient is stable; otherwise, use left anterolateral thoracotomy. |
| Equivocal | pericardial window or formal transthoracic echocardiography (TTE) is recommended. |
| Negative | close clinical monitoring or discharge is recommended, according to clinical suspicion for injury. |
| Abdominal FAST (blunt abdominal trauma) | |
| Positive | in the unstable patient, emergent exploratory laparotomy is recommended. In a stable patient, cross-sectional imaging (CT scan) is recommended. |
| Equivocal | in the unstable patient, diagnostic peritoneal aspiration (DPA) is recommended. In a stable patient, cross-sectional imaging (CT scan) is recommended. |
| Negative | in the unstable patient, diagnostic peritoneal aspiration (DPA) is recommended if clinical suspicion for intra-abdominal bleeding exists. In a stable patient, a CT scan, close clinical monitoring, or discharge is recommended, according to clinical suspicion for injury. |
NB!
- Repeating FAST while preparing to perform diagnostic peritoneal aspiration is useful to quickly reassess unstable patients with blunt abdominal trauma with initially negative FAST. Intra-abdominal hemorrhage may not be significant enough on presentation to be FAST-positive initially.
- Be cautious if pericardial FAST is negative in patients with penetrating thoracic trauma, especially if unstable. Cardiac injuries can decompress through the injured pericardium, most commonly into the left hemithorax, resulting in negative pericardial FAST. Therefore, unstable patients with this mechanism of injury and FAST finding should undergo a chest x-ray. If it reveals a hemothorax, a chest tube must be placed. Ongoing or high-volume chest tube output in this clinical context may be from a cardiac injury.
- If the pericardial fluid is seen in the subxiphoid view, surgical intervention is warranted.
- If intra-abdominal fluid is seen in any of the three abdominal views, emergent laparotomy is indicated in unstable patients.
- Stable patients with intra-abdominal fluid should proceed to cross-sectional imaging.
More recently, thoracic views have been added to the FAST exam and termed eFAST. These windows assess the chest bilaterally for pneumo- and hemothorax. In some series, the reported sensitivities of eFAST (86–100%) are superior to that of chest x-ray (27–83%) in the detection of pneumothoraces (Governatori 2015, Nandipati 2011, Wilkerson 2010).
The extended FAST (eFAST) has entered into clinical practice with the addition of bilateral thoracic views to assess for pneumo- and hemothorax.
Negative FAST does not exclude injury. Ultrasound is user-dependent; therefore, clinicians should be cautious in interpreting negative FAST. Sensitivities of abdominal and suprapubic views in FAST vary widely, with ranges of 22–98% reported in recent literature
If clinical suspicion for injury persists despite negative FAST, FAST should be repeated, additional investigations should be performed, or intervention should be pursued, depending on patient’s clinical condition.
.
Literature
- Rozycki GS, Ochsner MG, Jaffin JH, Champion HR. Prospective evaluation of surgeons’ use of ultrasound in the evaluation of trauma patients. J Trauma. 1993 Apr;34(4):516-26.
- Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998 Oct;228(4):557-567.
- Rozycki GS, Ochsner MG, Schmidt JA, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995 Sep;39(3):492-8.
- Rozycki GS, Feliciano DV, Ochsner MG, et al. The Role of Ultrasound in Patients with Possible Penetrating Cardiac Wounds: A Prospective Multicenter Study. J Trauma. 1999 Apr;46(4):543-51.
- Richards JR, McGahan JP. Focused Assessment with Sonography in Trauma (FAST) in 2017: What Radiologist Can Learn. Radiology. 2017 Apr;283(1):30-48.
- Ball CG, Williams BH, Wyrzykowski AD, et al. A Caveat to the Performance of Pericardial Ultrasound in Patients with Penetrating Cardiac Wounds. J Trauma. 2009 Nov;67(5):1123-4.
- Nandipati KC, Allamaneni S, Kakarla R, et al. Extended Focused Assessment with Sonography for Trauma (EFAST) in the Diagnosis of Pneumothorax: Experience at a Community Based Level I Trauma Center. Injury. 2011 May;42(5):511-4.
- Governatori NJ, Saul T, Siadecki SD, et al. Ultrasound in the Evaluation of Penetrating Thoraco-Abdominal Trauma: A Review of the Literature. Med Ultrason. 2015 Dec;17(4):528-34.
- Wilkerson RG, Stone MB. Sensitivity of Bedside Ultrasound and Supine Anteroposterior Chest Radiographs for the Identification of Pneumothorax After Blunt Trauma. Acad Emerg Med. 2010 Jan;17(1):11-7.
- Matsushima K, Khor D, Berona K, Antoku D, Dollbaum R, Khan M, Demetriades D. Double Jeopardy in Penetrating Trauma: Get FAST, Get It Right. World J Surg. 2017 Aug 4. [Epub ahead of print]
- Carter JW, Falco MH, Chopko MS, Flyn WJ Jr, Wiles Iii CE, Guo WA. Do we really rely on fast for decision-making in the management of blunt abdominal trauma?. Injury. 2015 May;26(5):817-21.
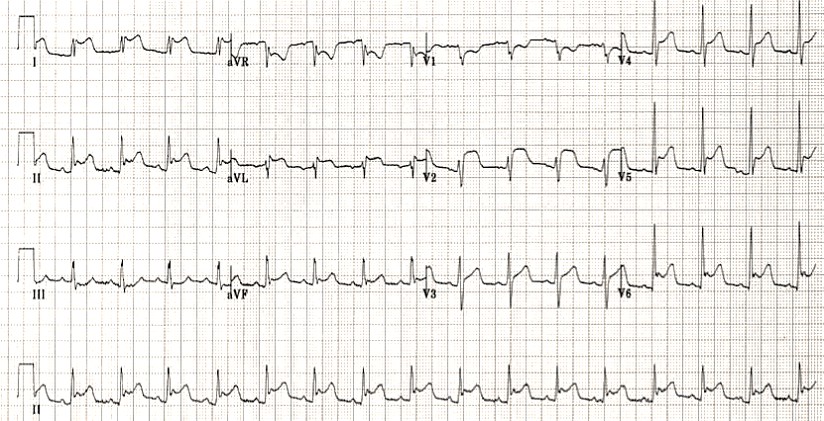
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
National Institutes of Health Stroke Scale (NIHSS) – Online calculator
The National Institutes of Health Stroke Scale (NIHSS) is a scale designed to assess the…
Charlson Comorbidity Index (CCI) Online Calculator
Charlson Comorbidity Index predicts 10-year survival in patients with multiple comorbidities.
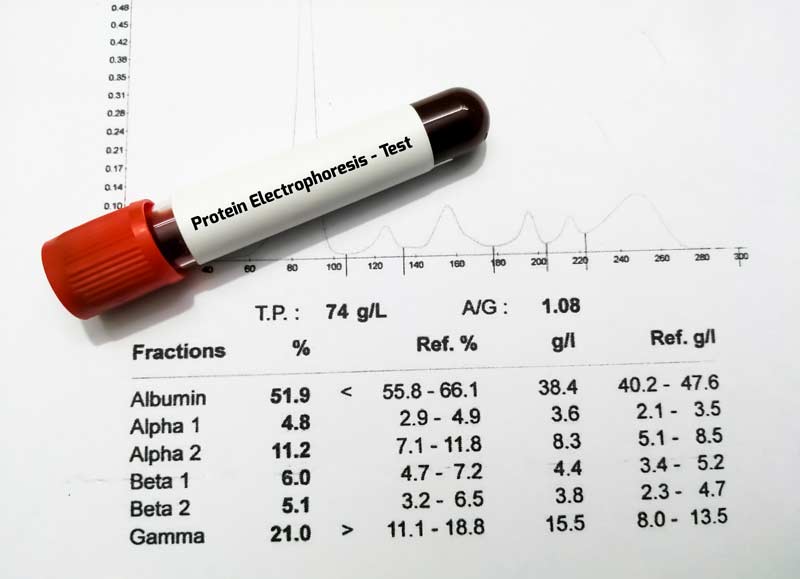
Multiple Myeloma Diagnostic Criteria – Online Calculator
Revised Multiple Myeloma International Staging System (R-ISS) Online Calculator
Revised Multiple Myeloma International Staging System (R-ISS) – prognostication tool for myeloma patients based on…
Multiple Myeloma International Staging System (ISS) Online Calculator
Multiple Myeloma International Staging System (ISS) prognosticates the severity of multiple myeloma based on routinely…