POSSUM for Operative Morbidity and Mortality Risk – Online Calculator

POSSUM calculates the risk of surgical morbidity and mortality, which can be used to help patients and their families make informed decisions about surgery.
POSSUM for Operative Morbidity and Mortality Risk can be used in patients undergoing emergency and elective general surgical procedures. Risk estimates can help patients and family members in the process of informed consent and in management of expectations.
The Physiological and Operating Severity Scale for Mortality and Morbidity (POSSUM) estimates morbidity and mortality in general surgery.
It can be used for both emergency and planned surgery. The POSSUM should be calculated when the decision to operate is made. The percentages can be shared with the patient when discussing the risks of the operation.
To score on the POSSUM scale is an addition of selected points.
Physiological score and operation severity score are weighted differently.
| Assessment parameter | Points | |
| Physiological score | ||
| Age, years | ≤60 | 1 |
| 61-70 | 2 | |
| ≥71 | 4 | |
| Cardiac | No failure | 1 |
| Diuretic, digoxin or angina/hypertension meds | 2 | |
| Peripheral edema, warfarin, or borderline cardiomegaly on chest X-ray (CXR) | 4 | |
| Raised jugular venous pressure, or cardiomegaly on CXR | 8 | |
| Respiratory | No dyspnea | 1 |
| Exertional dyspnea or mild COPD on CXR | 2 | |
| Limiting dyspnea or moderate COPD on CXR | 4 | |
| Dyspnea at rest or fibrosis/consolidation on CXR | 8 | |
| sBP mm Hg Norm: 100-120 mm Hg | ≤89 | 8 |
| 90-99 | 4 | |
| 100-109 | 2 | |
| 110-130 | 1 | |
| 131-170 | 2 | |
| ≥171 | 4 | |
| HR, beats/min Norm: 60-100, beats/min | ≤39 | 8 |
| 40-49 | 2 | |
| 50-80 | 1 | |
| 81-100 | 2 | |
| 101-120 | 4 | |
| ≥121 | 8 | |
| Glasgow Coma Scale | 15 | 1 |
| 12-14 | 2 | |
| 9-11 | 4 | |
| ≤8 | 8 | |
| Hemoglobin Norm: 120-170 g/L (12-17 g/dL) | ||
| g/L | g/dL | |
| 130-160 | 13-16 | 1 |
| 115-129 | 11.5-12.9 | 2 |
| 161-170 | 16.1-17.0 | 2 |
| 100-114 | 10.0-11.4 | 4 |
| 171-180 | 17.1-18.0 | 4 |
| ≤ 99 | ≤ 9.9 | 8 |
| ≥181 | ≥18.1 | 8 |
| WBC Norm: 3,7-10,7×103 cells/µL (3,7-10,7×109 cells/L) | 4-10 | 1 |
| 10.1-20.0 | 2 | |
| 3.1-4.0 | 2 | |
| ≥20.1 | 4 | |
| ≤3.0 | 4 | |
| BUN Norm: 2,9-7,1 mmol/L (8-20 mg/dL) | ||
| mg/dL | mmol/L | |
| ≤ 45 | ≤7.5 | 1 |
| 46-60 | 7.6-10.0 | 2 |
| 61-90 | 10.1-15.0 | 4 |
| ≥90 | ≥15.1 | 8 |
| Sodium Norm: 136-145 mmol/L (136-145 mEq/L) | ≥136 | 1 |
| 131-135 | 2 | |
| 126-130 | 4 | |
| ≤125 | 8 | |
| Potassium Norm: 3,5-5 mmol/L (3,5-5 mEq/L) | 3.5-5.0 | 1 |
| 3.2-3.4 | 2 | |
| 5.1-5.3 | 2 | |
| 2.9-3.1 | 4 | |
| 5.4-5.9 | 4 | |
| ≤2.8 | 8 | |
| ≥6.0 | 8 | |
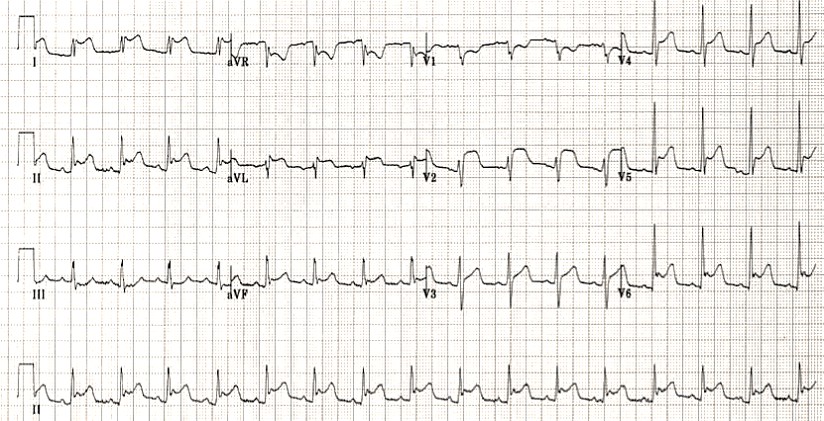
| ECG | Normal | 1 |
| Atrial fibrillation (HR 60-90) | 4 | |
| Any other abnormal rhythm, or 5 ectopic beats/min, Q waves or ST/T wave changes | 8 | |
| Operative severity score | ||
| Operative severity | Minor | 1 |
| Moderate (appendectomy, cholecystectomy, mastectomy, transurethral resection of the prostate) | 2 | |
| Major (laparotomy, bowel resection, cholecystectomy w choledochotomy, peripheral vascular procedure or major amputation) | 4 | |
| Major+ (aortic procedure, abdominoperineal resection, pancreatic or liver resection, esophagogastrectomy) | 8 | |
| Number of procedures | 1 | 1 |
| 2 | 4 | |
| >2 | 8 | |
| Estimated blood loss, ml | ||
| ≤100 | 1 | |
| 101-500 | 2 | |
| 501-999 | 4 | |
| ≥1000 | 8 | |
| Peritoneal soiling | None | 1 |
| Minor (serous fluid) | 2 | |
| Local pus | 4 | |
| Free bowel content, pus or blood | 8 | |
| Presence of malignancy Diagnosed before or during surgery | None | 1 |
| Primary only | 2 | |
| Lymph node mets | 4 | |
| Distant mets | 8 | |
| Mode of surgery | Elective | 1 |
| Emergency (within 24h), resuscitation >2h possible | 4 | |
| Emergency (within 2h) | 8 |
Severity of surgeries:
- Moderate: appendectomy, cholecystectomy, mastectomy, TURP
- Major: laparotomy, bowel resection, cholecystectomy w choledochotomy, peripheral vascular procedure or major amputation
- Major+: aortic procedure, abdominoperineal resection, pancreatic or liver resection, esophagogastrectomy
The POSSUM morbidity and mortality formulas are shown below:
- Morbidity ln[R/(1-R)] = – 5,91 + (0,16 x Physiological score) + (0,19 x operation severity score) (P<0,001).
- Mortality ln [R/(1 –R)] = -7,04+ (0,13 x Physiological score) + (0,16 x operation severity score) (P <0,001).
Predicied versus observed rates for mortality and morbidity*
| Predicted risk (%) | Mortality | Morbidity |
| 85 | 86.5 | 84.3 |
| 75 | 78.3 | 75.7 |
| 65 | 67.7 | 67.3 |
| 55 | 56.4 | 56.9 |
| 45 | 46.0 | 47.5 |
| 35 | 38.5 | 37.4 |
| 25 | 29.3 | 26.4 |
Morbidity was defined as any of the following:
- Wound haemorrhage: local haematoma requiring evacuation
- Deep haemorrhage: postoperative bleeding requiring re-exploration
- Chest infection: production of purulent sputum with positive
bacteriological cultures, with or without chest radiography changes or pyrexia, or consolidation seen on chest radiograph
- Woundinfection: wound cellulitis or the discharge ofpurulent exudate
- Urinary infection: the presence of z lo5 bacteria/ml with the presence of white cells in the urine, in previously clear urine
- Deep infection: the presence of an intra-abdominal collection confirmed clinically or radiologically.
- Septicaemia: positive blood culture
- Pyrexia of unknown origin: any temperature above 37°C for more than 24 h occurring after the original pyrexia following surgery (if present) had settled, for which no obvious cause could be found
- Wound dehiscence: superficial or deep wound breakdown
- Deep venous thrombosis and pulmonary embolus: when suspected, confirmed radiologically by venography or ventilation/perfusion scanning, or diagnosed at post mortem
- Cardiac failure: symptoms or signs of left ventricular or congestive cardiac failure which required an alteration from preoperative therapeutic measures
- Impaired renal function: arbitrarily defined as an increase in blood urea of > 5 mmol/l from preoperative levels
- Hypotension: a fall in systolic blood pressure below 90 mmHg for more than 2 h as determined by sphygmomanometry or arterial pressure transducer measurement
- “Any other complication”
The POSSUM was originally developed by Copeland and colleagues in 1991 to assess quality of care and provide a scoring system for surgical audit. Physiological and operative severity score data were obtained from 1,372 patients.
The original POSSUM was modified to the Portsmouth POSSUM, or P-POSSUM, in 1998 by Prytherch and colleagues, who derived a more accurate prediction for the mortality component.
Both the POSSUM and P-POSSUM slightly overestimate both morbidity and mortality.
Since the original publication of POSSUM, the score has been modified and validated for numerous subtypes of surgeries and clinical scenarios, including:
- Colorectal surgery
- Vascular surgery
- Oncologic gastric surgery
- Hepatectomy
- Emergency laparotomy
- Orthopedic surgery
The original POSSUM was modified by researchers in Portsmouth who derived a more accurate prediction of mortality, and the P-POSSUM model is now more commonly used to calculate the mortality component.
The POSSUM data set excludes trauma patients, so POSSUM should NOT be used to predict morbidity and mortality after trauma surgery.
The POSSUM should NOT dictate the decision to operate, which is a clinical decision.
Physiological score should be calculated at the time of surgery, not at the time of admission.
The definitions of surgical procedures are guidelines only. Not all procedures are listed, and the closest approximation should be selected.
The POSSUM may overestimate risk in hepatopancreaticobiliary surgery.
Similar / alternative tools:
- There are procedure-specific models for colorectal surgery (CR-POSSUM), vascular surgery (Vascular-POSSUM), and esophagogastric surgery (O-POSSUM, O for oesophagogastric).
- APACHE II is a similar assessment tool but is applied to intensive care patients and only assesses the risk of mortality.
- The Surgical Apgar Score (SAS) offers similar estimates for morbidity and mortality.
- The POSSUM is more comprehensive than the SAS (which is calculated based on 3 parameters), but the SAS is more objective.
- The SAS uses intraoperative parameters exclusively, whereas the POSSUM uses preoperative parameters.
- The ACS NSQIP risk calculator is a newer, similar assessment. It has not yet been as rigorously validated as the POSSUM.
- Other disease-specific scores may be used to assess risk, e.g. Revised Cardiac Risk Index for Pre-Operative Risk.
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Literature
- Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg 1991;78(3):355-60. https://pubmed.ncbi.nlm.nih.gov/2021856/
- Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg 1998 Sep;85(9):1217-20. https://pubmed.ncbi.nlm.nih.gov/9752863/
- Ramkumar T, Ng V, Fowler L, Farouk R. A comparison of POSSUM, P-POSSUM and colorectal POSSUM for the prediction of postoperative mortality in patients undergoing colorectal resection. Dis Colon Rectum. 2006 Mar;49(3):330-5. https://pubmed.ncbi.nlm.nih.gov/16421662/
- Tez M, Yoldaş O, Gocmen E, Külah B, Koc M. Evaluation of P-POSSUM and CR-POSSUM scores in patients with colorectal cancer undergoing resection. World J Surg. 2006 Dec;30(12):2266-9. https://pubmed.ncbi.nlm.nih.gov/17103102/
- Lam CM, Fan ST, Yuen AW, Law WL, Poon K. Validation of POSSUM scoring systems for audit of major hepatectomy. Br J Surg. 2004 Apr;91(4):450-4. https://pubmed.ncbi.nlm.nih.gov/15048745/
- Mohil RS, Bhatnagar D, Bahadur L, Rajneesh, Dev DK, Magan M. POSSUM and P-POSSUM for risk-adjusted audit of patients undergoing emergency laparotomy. Br J Surg. 2004 Apr;91(4):500-3. https://pubmed.ncbi.nlm.nih.gov/15048756/
- van Zeeland ML, Genovesi IP, Mulder JW, Strating PR, Glas AS, Engel AF. POSSUM predicts hospital mortality and long-term survival in patients with hip fractures. J Trauma. 2011 Apr;70(4):E67-72. https://pubmed.ncbi.nlm.nih.gov/21613973/
- Chen T, Wang H, Wang H, Song Y, Li X, Wang J. POSSUM and P-POSSUM as predictors of postoperative morbidity and mortality in patients undergoing hepato-biliary-pancreatic surgery: a meta-analysis. Ann Surg Oncol. 2013 Aug;20(8):2501-10. https://pubmed.ncbi.nlm.nih.gov/23435569/
- Copeland GP. The POSSUM System of Surgical Audit. Arch Surg. 2002;137(1):15-19. doi:10.1001/archsurg.137.1.15. http://jamanetwork.com/journals/jamasurgery/fullarticle/212013
Karnofsky Performance Status Scale Online Calculator
Karnofsky performance status scale determines ability of patient to tolerate chemotherapy. For patients ≥ 16…
Drug Resistance in Pneumonia (DRIP) Score. Online Calculator
The purpose of the DRIP score is to determine when broad-spectrum antibiotics should be used…
Focused Assessment with Sonography for Trauma (FAST): Online Calculator
Focused Assessment with Sonography for Trauma (FAST) predicts the presence of pericardial or intra-abdominal injury…
Interactive OSCE Checklist – Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents
Maximum Allowable Blood Loss (ABL) Without Transfusion: Online calculator
Maximum Allowable Blood Loss (ABL) Without Transfusion formula can be used in patients with blood…
Revised Cardiac Risk Index for Pre-Operative Risk (RCRI) Online Calculator
The revised cardiac risk index for preoperative risk may be used in patients ≥45 years…