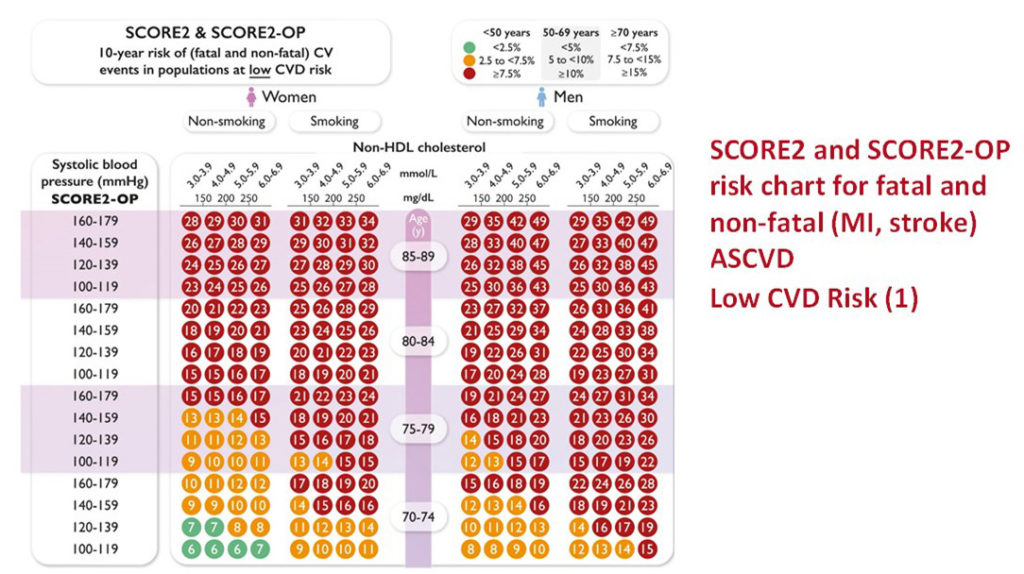
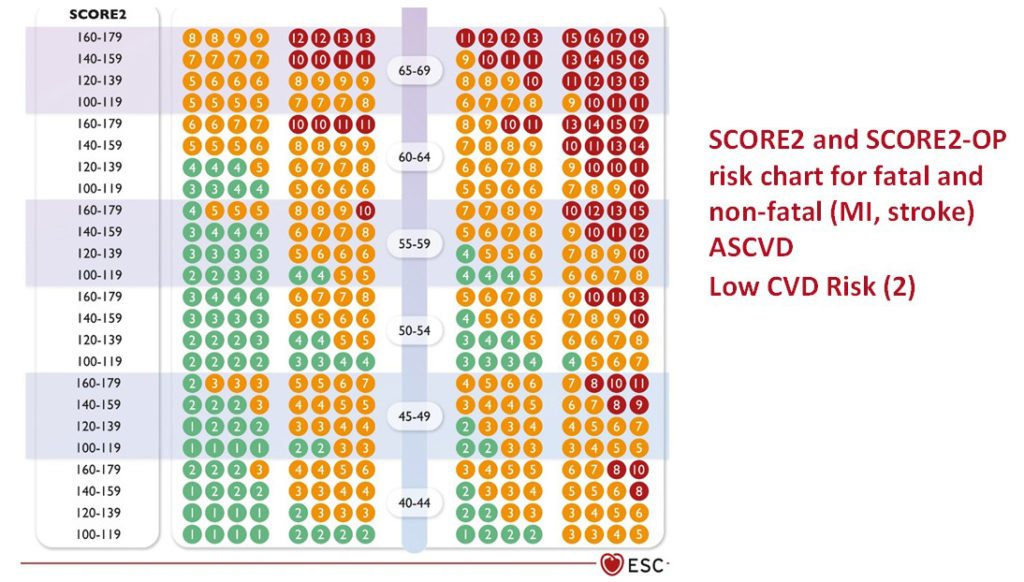
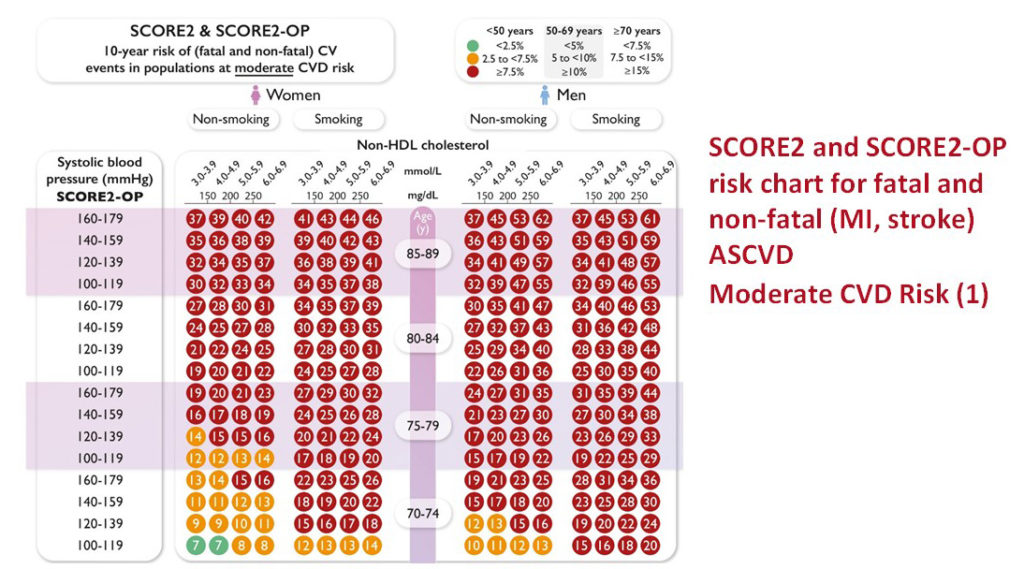
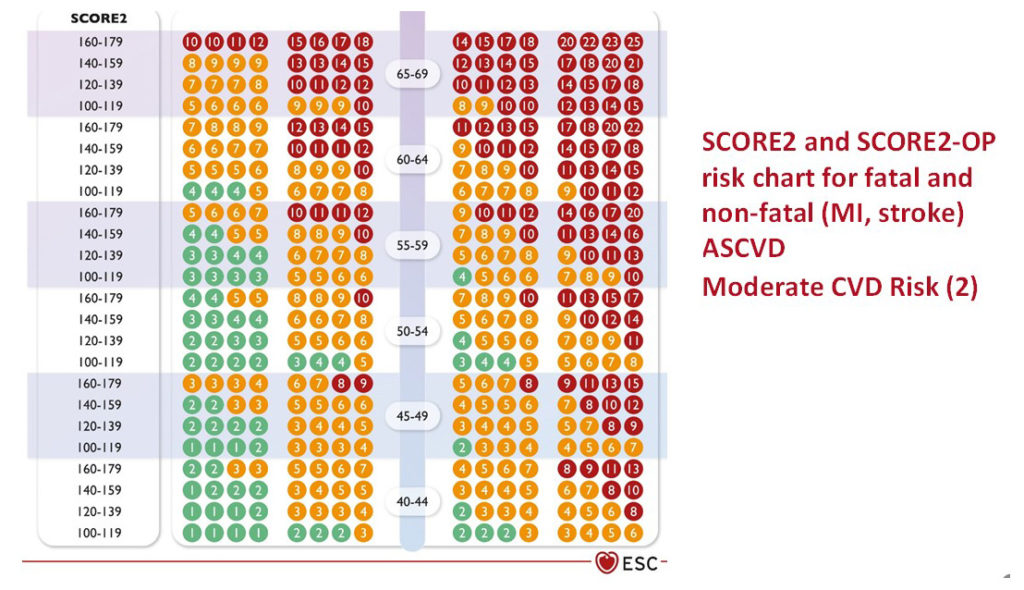
SCORE2 and SCORE2-OP scales for determining cardiovascular risk

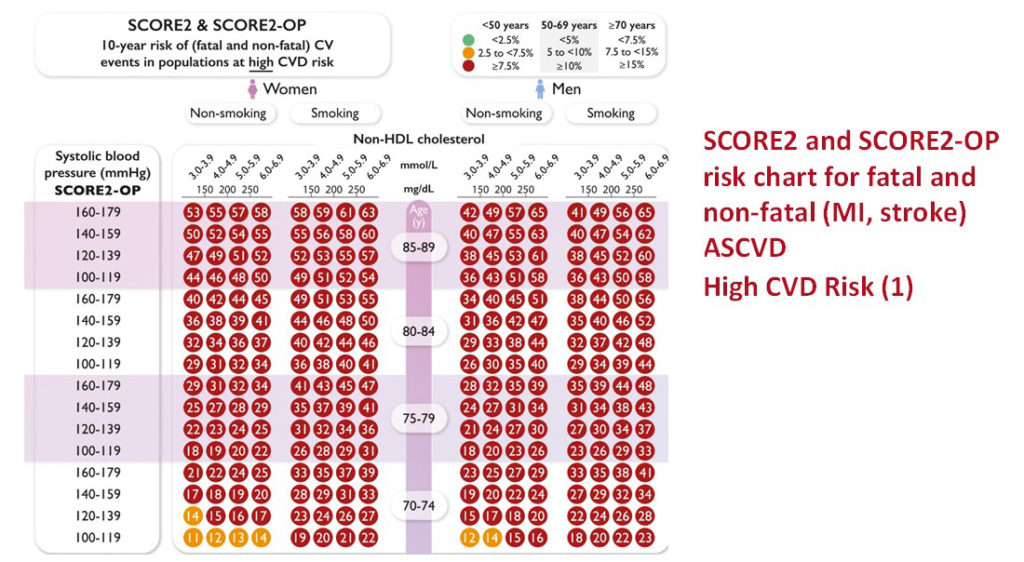
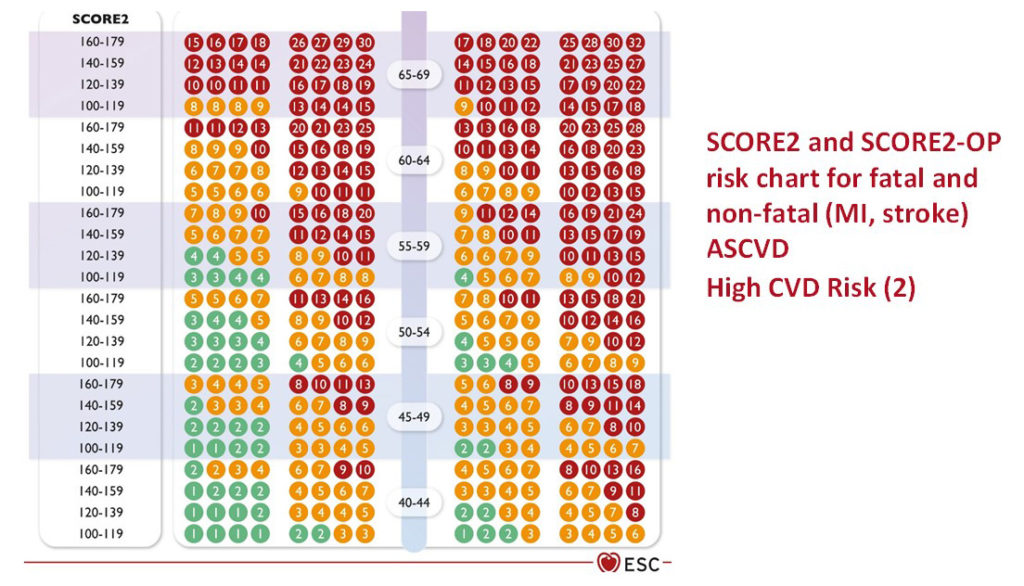
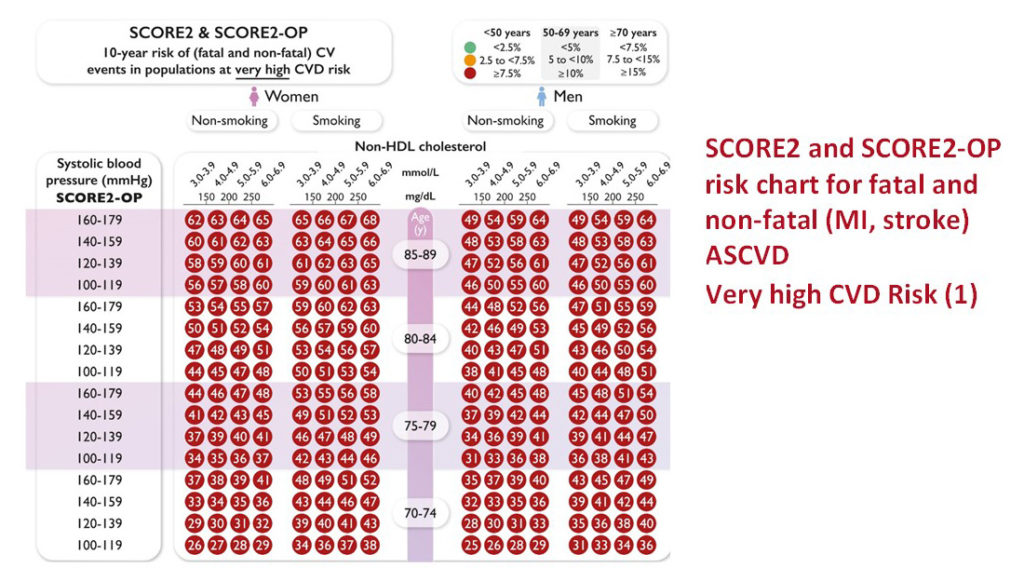
Apparently healthy people are those without established ASCVD, type 2 DM, or severe comorbidities. In the 2016 ESC prevention guidelines, the Systemic Coronary Risk Estimation (SCORE) algorithm was used to estimate 10-year risk of CVD death. However, CVD morbidity (non-fatal myocardial infarction, non-fatal stroke) combined with CVD mortality better reflects the total burden of ASCVD. The updated SCORE algorithm – SCORE2 – used in these guidelines, estimates an individual’s 10-year risk of fatal and non-fatal CVD events (myocardial infarction, stroke) in apparently healthy people aged 40–69 years with risk factors that are untreated or have been stable for several years.
NB! The SCORE2 charts do not apply to persons with documented CVD or other high-risk conditions such as DM, FH, or other genetic or rare lipid or BP disorders, CKD, and in pregnant women.
Several specific considerations apply to CVD risk estimation in older people.
First, the gradient of the relationship between classical risk factors, such as lipids and BP, with CVD risk attenuates with age.
Second, CVD-free survival dissociates from overall survival progressively with increasing age, because risk for non-CVD mortality increases (‘competing risk’). For these reasons, traditional risk models that do not take into account the competing risk of non-CVD mortality, tend to overestimate the actual 10-year risk of CVD, and hence overestimate the potential benefit of treatment. The SCORE2-OP algorithm estimates 5-year and 10-year fatal and non-fatal CVD events (myocardial infarction, stroke) adjusted for competing risks in apparently healthy people aged ≥70 years.
Algorithm of use
To estimate a person’s 10-year risk of total CVD events, one must first identify the correct cluster of countries and the accompanying risk table for their sex, smoking status, and (nearest) age. Within that table, one then finds the cell nearest to the person’s BP and non-HDL-C. Risk estimates then need to be adjusted upwards as the person approaches the next age category.
SCORE2 & SCORE2-OP in populations at low CVD risk:
SCORE2 & SCORE2-OP in populations at moderate CVD risk:
SCORE2 & SCORE2-OP in populations at high CVD risk:
SCORE2 & SCORE2-OP in populations at very high CVD risk:
ASCVD = atherosclerotic cardiovascular disease; CV = cardiovascular; CVD = cardiovascular disease; SBP = systolic blood pressure; HDL-C = high-density lipoprotein cholesterol; SCORE2 = Systematic Coronary Risk Estimation 2; SCORE2-OP = Systematic Coronary Risk Estimation 2-Older Persons.
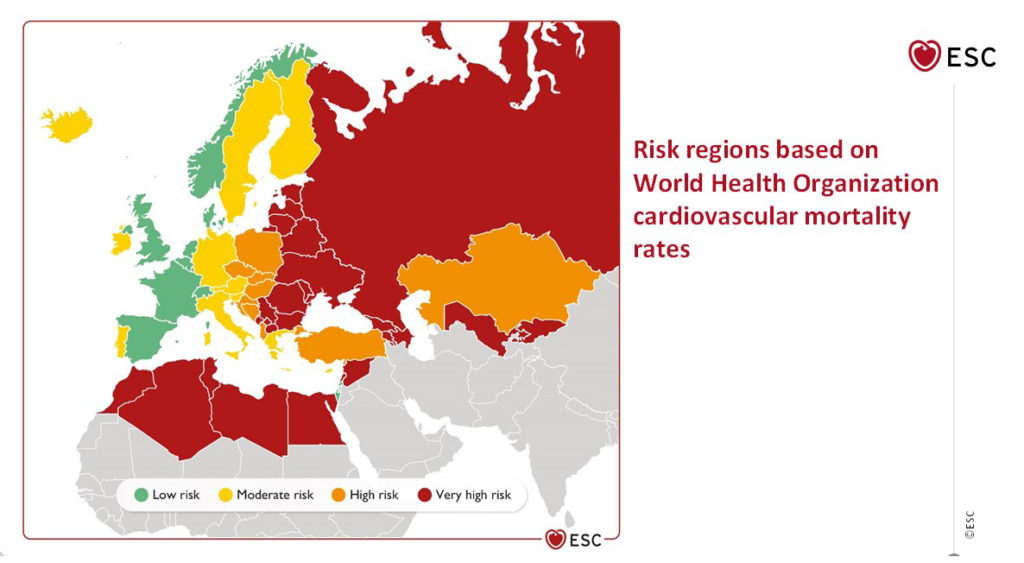
Risk regions based on World Health Organisation cfrdiovascular mortality rates
Low-risk countries: Belgium, Denmark, France, Israel, Luxembourg, Norway, Spain, Switzerland, the Netherlands, and the United Kingdom.
Moderate-risk countries: Austria, Cyprus, Finland, Germany, Greece, Iceland, Ireland, Italy, Malta, Portugal, San Marino, Slovenia, and Sweden.
High-risk countries: Albania, Bosnia and Herzegovina, Croatia, Czech Republic, Estonia, Hungary, Kazakhstan, Poland, Slovakia, and Turkey.
Very-high-risk countries: Algeria, Armenia, Azerbaijan, Belarus, Bulgaria, Egypt, Georgia, Kyrgyzstan, Latvia, Lebanon, Libya, Lithuania, Montenegro, Morocco, Republic of Moldova, Romania, Russian Federation, Serbia, Syria, The Former Yugoslav Republic (Macedonia), Tunisia, Ukraine, and Uzbekistan.
A source:
Frank L J Visseren, François Mach, Yvo M Smulders, David Carballo, Konstantinos C Koskinas, Maria Bäck, Athanase Benetos, Alessandro Biffi, José-Manuel Boavida, Davide Capodanno, Bernard Cosyns, Carolyn Crawford, Constantinos H Davos, Ileana Desormais, Emanuele Di Angelantonio, Oscar H Franco, Sigrun Halvorsen, F D Richard Hobbs, Monika Hollander, Ewa A Jankowska, Matthias Michal, Simona Sacco, Naveed Sattar, Lale Tokgozoglu, Serena Tonstad, Konstantinos P Tsioufis, Ineke van Dis, Isabelle C van Gelder, Christoph Wanner, Bryan Williams, ESC Scientific Document Group, 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC), European Heart Journal, Volume 42, Issue 34, 7 September 2021, Pages 3227–3337, https://doi.org/10.1093/eurheartj/ehab484
Register on our website right now to have access to more learning materials!
Subscribe to our pages:
Baseline Cardiovascular Risk Assessment in Cancer Patients Scheduled to Receive Cardiotoxic Cancer Therapies (Anthracycline Chemotherapy) – Online Calculator
Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies (Anthracycline Chemotherapy)…
SAVED VTE Score
SAVED score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…
IMPEDE VTE Score
IMPEDE score for venous thromboembolism risk stratification in patients with multiple myeloma receiving immunomodulators. [ezfc…
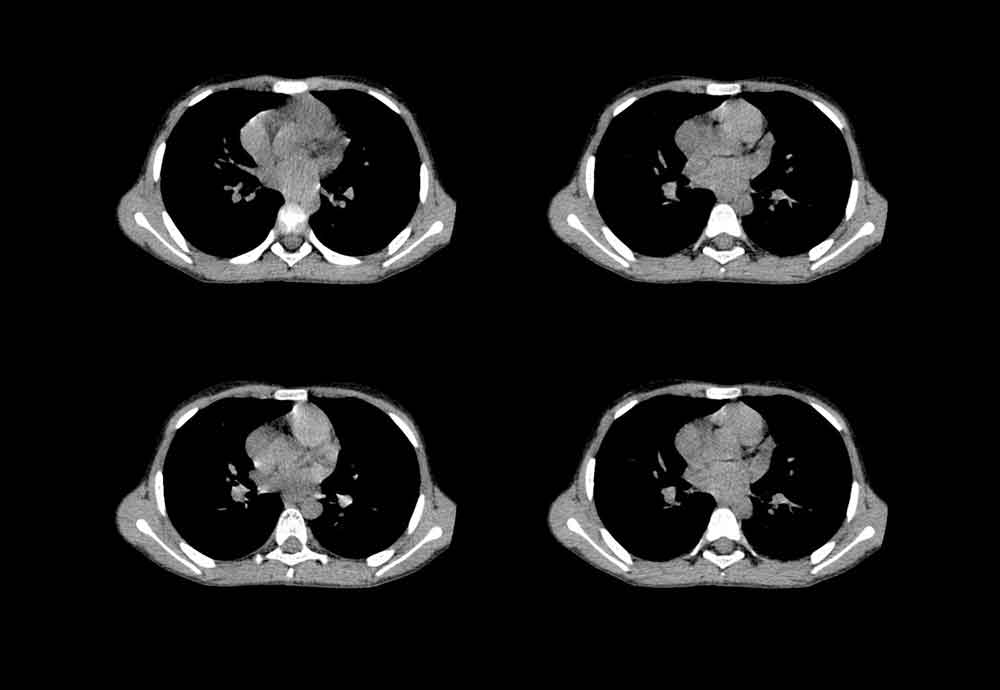
Chest CT Scan
To analyze a CT scan of the chest, imagine that the patient is lying on…
X-ray Heart Borders
According to the radiograph of the chest, the boundaries of the heart are formed: The…
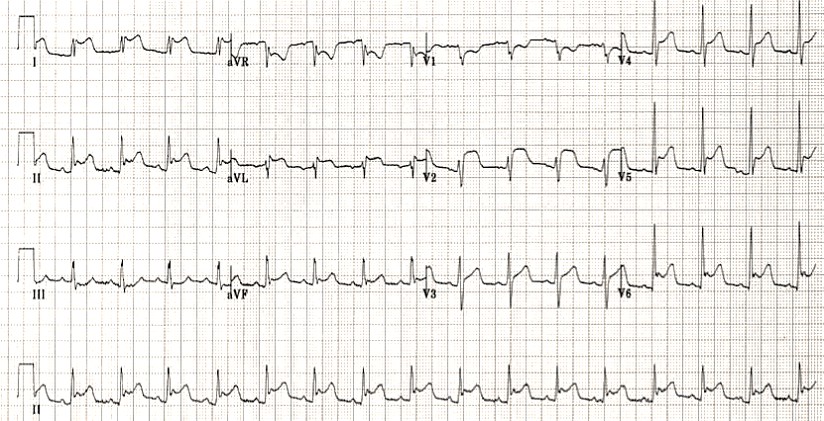
Emergency care of a patient with chest pain – Acute Coronary Syndrome with ST-segment elevation and equivalents /OSCE guide
Opening the consultationWash your hands and don PPE if appropriateIntroduce yourself to the patient including…